In recent years, the proliferation of online vendors offering Diazepam as a “research chemical” has raised significant concerns within the scientific community and among those interested in purchasing such substances. While these sellers may claim to provide a legitimate outlet for scientific research, a closer examination reveals numerous issues that warrant critical scrutiny.
First and foremost, the sale of Diazepam as a research chemical raises ethical and legal questions. Diazepam is a well-known prescription medication for anxiety and other medical conditions. It is not a designer drug or a novel research chemical. Selling it online under the guise of scientific research appears deceptive and potentially illegal in many jurisdictions.
Furthermore, the quality and safety of Diazepam purchased from these online vendors are highly questionable. Unlike regulated pharmaceuticals, these substances are not subject to stringent quality control standards, leaving buyers uncertain about the purity and potency of what they receive. This lack of oversight poses a significant risk to individuals who may inadvertently purchase adulterated or misrepresented products.
Moreover, the motivations of these sellers often come into question. While they claim to cater to the scientific community, their marketing tactics and accessibility to the general public suggest otherwise. The ease with which one can buy Diazepam for sale online raises concerns about potential misuse and abuse, undermining the intended purpose of legitimate scientific research.
- 1 Summary
- 2 History and culture
- 3 Chemistry
- 4 Pharmacology
- 5 Subjective effects
- 6 Toxicity
- 7 Legal status
- 8 FAQ
- 8.1 1. What is Diazepam?
- 8.2 2. How does Diazepam work?
- 8.3 3. What conditions are typically treated with Diazepam?
- 8.4 4. Is Diazepam safe to use?
- 8.5 5. How should I take Diazepam?
- 8.6 6. What are the potential side effects of Diazepam?
- 8.7 7. Can Diazepam be addictive?
- 8.8 8. Can I drink alcohol while taking Diazepam?
- 8.9 9. How long can I take Diazepam?
- 8.10 10. Is driving or operating heavy machinery safe while taking Diazepam?
- 8.11 11. Can I take Diazepam during pregnancy or while breastfeeding?
- 9 References
Summary
Diazepam, also recognized as Valium belongs to the benzodiazepine class of depressant substances. Its primary mode of action involves augmenting the impact of the inhibitory neurotransmitter known as GABA.
Initially patented in 1955 by the pharmaceutical firm Hoffman-La Roche, Diazepam has remained one of the most frequently prescribed medications globally since its introduction in 1963. Its versatile applications encompass the treatment of various conditions, including anxiety, panic attacks, insomnia, seizures, muscle spasms, and restless legs syndrome. Notably, Diazepam is pivotal in the World Health Organization’s Essential Drugs List, which outlines the fundamental pharmaceutical requirements for a basic healthcare system.
Subjectively, Diazepam induces effects such as alleviating anxiety, causing sedation, and promoting muscle relaxation. It stands out for its rapid onset of action compared to other benzodiazepines, even though it generally offers fewer recreational effects than counterparts like clonazepam (Klonopin) and alprazolam (Xanax).
While Diazepam has relatively low toxicity, it bears a moderate potential for abuse and can lead to physical and psychological dependence with prolonged usage. Moreover, combined with alcohol, opiates, or other depressants, it may result in respiratory depression, which can be fatal. Consequently, responsible use and adherence to harm reduction practices are strongly recommended when dealing with this substance.
It is crucial to note that abrupt discontinuation of benzodiazepines can pose significant risks, potentially endangering individuals who have been using them regularly for extended periods. This can lead to seizures or even fatal outcomes. Therefore, adopting a gradual tapering approach is highly advisable, progressively reducing the daily dosage over an extended period rather than abruptly ceasing use.
Furthermore, there is speculation that Diazepam may have a natural origin, as it has been discovered in various plant and animal organisms.
| Identifiers | |
|---|---|
| show IUPAC name | |
| CAS Number | 439-14-5 |
| PubChem CID | 3016 |
| IUPHAR/BPS | 3364 |
| DrugBank | DB00829 |
| ChemSpider | 2908 |
| UNII | Q3JTX2Q7TU |
| KEGG | D00293 |
| ChEBI | CHEBI:49575 |
| ChEMBL | ChEMBL12 |
| CompTox Dashboard (EPA) | DTXSID4020406 |
| ECHA InfoCard | 100.006.476 |
| Chemical and physical data | |
| Formula | C16H13ClN2O |
| Molar mass | 284.74 g·mol−1 |
History and culture
After the approval of chlordiazepoxide (Librium) in 1960, diazepam emerged as the second benzodiazepine, conceived by Leo Sternbach of the pharmaceutical company Hoffman-La Roche. It debuted in 1963, positioning itself as an enhanced iteration of Librium. Diazepam swiftly gained widespread popularity, eclipsing Librium in sales and propelling Roche into the ranks of pharmaceutical industry giants. Following this initial success, other pharmaceutical companies ventured into developing various benzodiazepine derivatives.
The benzodiazepines earned favour among medical practitioners as an advancement over barbiturates, which possessed a relatively narrow therapeutic range and induced more pronounced sedation at therapeutic dosages. Moreover, benzodiazepines proved significantly safer; fatal outcomes from diazepam overdoses were rare, except when combined with substantial quantities of other depressants, such as alcohol or opioids. Initially, benzodiazepine drugs like diazepam garnered significant public support. However, this sentiment evolved over time into one marked by growing criticism and calls for stricter prescription regulations.
Roche, in collaboration with the William Douglas McAdams Agency under the guidance of Arthur Sackler, vigorously marketed diazepam. It became the top-selling pharmaceutical in the United States between 1969 and 1982, with its zenith in 1978 when 2.3 billion Valium tablets were sold. While psychiatrists still prescribe diazepam for the short-term alleviation of anxiety, the field of neurology has assumed a prominent role in prescribing diazepam for palliative treatment in specific epilepsy and spastic conditions.
Chemistry
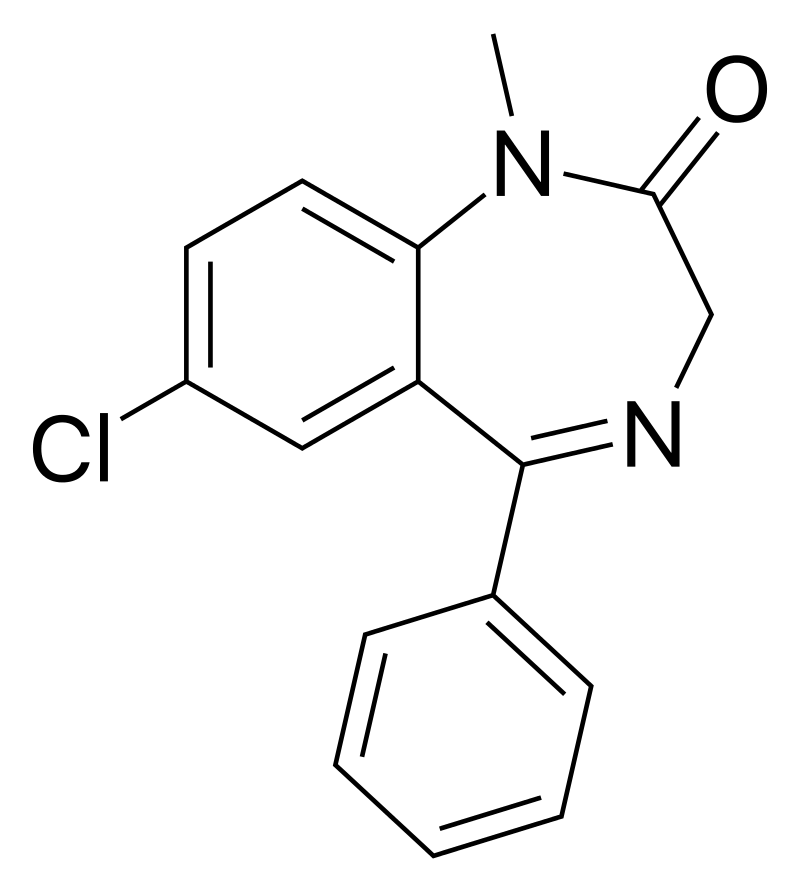
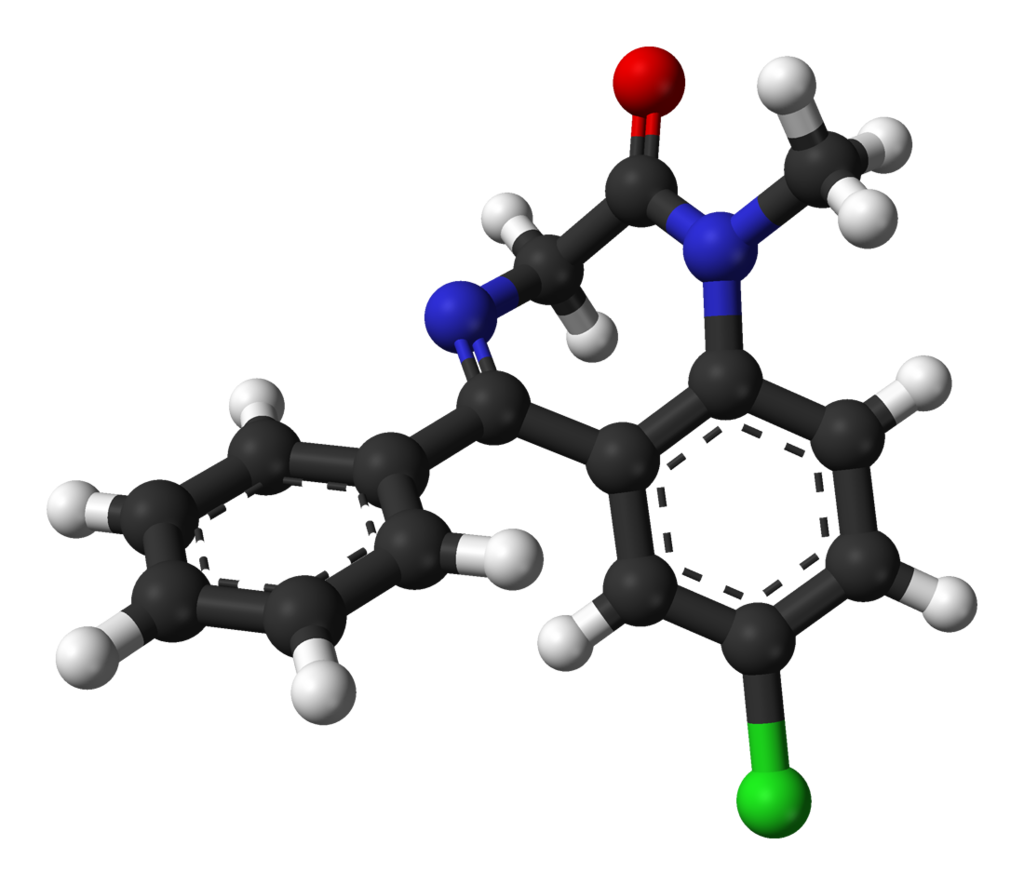
Diazepam belongs to the benzodiazepine drug class, characterized by a benzene ring fused to a diazepine ring, forming a seven-membered ring structure with nitrogen atoms at positions R1 and R4. At R1, Diazepam features a methyl group substitution. Additionally, the benzodiazepine ring is connected at R5 to an aromatic phenyl ring. The benzyl ring at R7 carries a chlorine group within the bicyclic core. Furthermore, Diazepam includes an oxygen group double-bonded to R2 of its diazepine ring, resulting in a ketone formation. This oxygen substitution at R2 is a shared characteristic among benzodiazepine drugs bearing the suffix “-azepam.”
Diazepam is classified as a 1,4-benzodiazepine and presents as solid white or yellow crystals with a melting point ranging from 131.5 to 134.5 °C. It possesses an odourless nature and a slightly bitter taste. The pH of Diazepam is neutral, with a value of 7. It is important to note that in its injectable form, Diazepam may contain additives like benzoic acid/benzoate. Consequently, it can potentially interact with plastics, making it unsuitable for storage in plastic containers, bottles, or syringes. The compound may leach into plastic bags and tubing for intravenous infusions. The degree of absorption depends on various factors, including temperature, concentration, flow rates, and tubing length. If a precipitate forms and does not dissolve, Diazepam should not be administered.
Pharmacology
Diazepam is a “classical” benzodiazepine with a long duration of action. These benzodiazepines exert their effects through binding to micromolar benzodiazepine binding sites, acting as calcium channel blockers. They significantly impede depolarization-sensitive calcium uptake in rat nerve cell preparations. In addition, diazepam inhibits acetylcholine release in mouse hippocampal synaptosomes. This inhibition has been observed by measuring sodium-dependent high-affinity choline uptake in mouse brain cells in vitro, following prior administration of diazepam to the mice in vivo. This mechanism may help elucidate diazepam’s anticonvulsant properties.
Benzodiazepines serve as positive allosteric modulators for GABA type A receptors (GABAA). GABAA receptors are ligand-gated chloride-selective ion channels activated by GABA, the principal inhibitory neurotransmitter in the brain. The binding of benzodiazepines to this receptor complex enhances GABA binding, subsequently increasing the overall conduction of chloride ions across the neuronal cell membrane. This heightened influx of chloride ions results in hyperpolarization of the neuron’s membrane potential. Consequently, the disparity between resting and threshold potential widens, making neuronal firing less likely. This reduces the arousal of the cortical and limbic systems within the central nervous system.
The GABAA receptor is a heteromer composed of five subunits, with the most common configuration being two αs, two βs, and one γ (α2β2γ). Multiple subtypes exist for each subunit (α1–6, β1–3, and γ1–3). GABAA receptors containing the α1 subunit mediate the sedative, anterograde amnesic, and, to some extent, anticonvulsive effects of diazepam. α2-containing receptors mediate the anxiolytic effects and, to a significant degree, the myorelaxant effects. α3 and α5-containing receptors also contribute to the myorelaxant effects of benzodiazepines, while α5-containing receptors modulate the temporal and spatial memory effects of benzodiazepines.
It’s worth noting that diazepam is not the sole drug that targets these GABAA receptors. Drugs like flumazenil also bind to GABAA receptors to induce their effects. Diazepam primarily acts on areas of the limbic system, thalamus, and hypothalamus, resulting in anxiolytic effects. Benzodiazepines, including diazepam, enhance inhibitory processes within the cerebral cortex.
Benzodiazepines exert various effects by binding to the benzodiazepine receptor site, amplifying the efficiency and impact of the neurotransmitter gamma-aminobutyric acid (GABA) through its receptors. As these receptors are the most prevalent inhibitory receptor set in the brain, their modulation leads to diazepam’s sedative and calming effects on the nervous system. Notably, the anticonvulsant properties of benzodiazepines may be, at least in part, attributable to their binding to voltage-dependent sodium channels rather than benzodiazepine receptors.
Subjective effects
Disclaimer: The effects listed below are based on anecdotal user reports and analyses of PsychonautWiki contributors and should be viewed with scepticism. The occurrence of these effects may not be predictable or reliable, but higher doses are more likely to induce a broader range of products. It is essential to note that adverse effects, including addiction, severe injury, or even death ☠, become more likely with higher doses.
Physical:
- Sedation: This drug induces a pronounced lethargy, making users feel overwhelmingly tired. Higher doses can lead to an extreme sense of sleep deprivation, causing users to feel as though they haven’t slept in days and compelling them to sit down, often leading to unconsciousness.
- Muscle Relaxation: Compared to alprazolam (Xanax), diazepam offers more extensive muscle relaxation.
- Motor Control Loss
- Respiratory Depression
- Dizziness
- Seizure Suppression
- Physical Euphoria: While diazepam typically suppresses emotions, some users report moderate to intense feelings of relaxation, pleasure, and physical comfort, especially in those with pre-existing anxiety. Notably, this effect may be more subtle than faster-acting benzodiazepines like alprazolam (Xanax).
Visual:
- Visual Acuity Suppression: Diazepam can cause blurred or suppressed visual acuity like many depressants. Though less common than other benzodiazepines, it may still occur at higher doses or in individuals with low tolerance.
Paradoxical:
- Paradoxical Reactions: Some individuals may experience paradoxical reactions to benzodiazepines, including increased seizures (in people with epilepsy), aggression, heightened anxiety, violent behaviour, impulse control loss, irritability, and suicidal tendencies. These effects are rare in the general population, with an incidence rate below 1%. They are more common in recreational users, individuals with mental disorders, children, and those on high-dosage regimens.
Cognitive:
- Head Space: The cognitive effects of diazepam are characterized by intense sedation and decreased inhibition. Prominent mental effects may include:
- Anxiety Suppression
- Disinhibition
- Delusions of Sobriety: A false belief of being perfectly sober despite obvious evidence to the contrary, often occurring at high doses.
- Thought Deceleration
- Analysis Suppression
- Amnesia
- Memory Suppression: Primarily affects short-term memory, leading to forgetfulness and disorganized behaviours.
- Compulsive Redosing
- Emotion Suppression: Besides reducing anxiety, diazepam dulls other emotions, though less intensely than antipsychotics.
- Motivation Suppression: Due to moderate sedation and lethargy, engaging in physical activities or high-effort tasks may become challenging, especially at higher doses.
- Language Suppression: Diazepam and most benzodiazepines can cause slurred speech and difficulty articulating words clearly.
After:
- Rebound Anxiety: Commonly observed with anxiety-relieving substances like benzodiazepines. It corresponds to the total duration under the substance’s influence and the total amount consumed, potentially leading to dependence and addiction.
- Dream Potentiation or Dream Suppression
- Residual Sleepiness: While benzodiazepines can aid in inducing sleep, their effects may linger the following morning, leaving users groggy or dull for a few hours.
- Thought Deceleration
- Thought Disorganization
- Irritability

Toxicity
Diazepam is characterized by its low toxicity when administered at appropriate doses. However, its potential for lethality escalates significantly when combined with depressants such as alcohol or opioids.
It is highly advisable to practice harm reduction techniques, such as employing volumetric dosing, when using this substance to ensure precise dosage administration.
Regarding lethal dosage, diazepam’s oral LD50 (lethal dose in 50% of the population) is approximately 720 mg/kg in mice and 1240 mg/kg in rats.[28] In 1978, D. J. Greenblatt and colleagues reported two cases of individuals who consumed 500 and 2000 mg of diazepam, resulting in moderate comas. Fortunately, these individuals were discharged within 48 hours without significant complications despite having elevated levels of diazepam and its metabolites, esmethyldiazepam, oxazepam, and temazepam (as confirmed by hospital samples and follow-up tests).
Although a diazepam overdose is typically not fatal when taken in isolation, it remains a medical emergency that demands immediate attention from healthcare professionals. Flumazenil (Anexate) is the antidote for diazepam overdose, but its use is reserved for severe respiratory depression or cardiovascular complications. Given that flumazenil is short-acting and the effects of diazepam can persist for days, multiple doses of flumazenil may be required, alongside artificial respiration and cardiovascular stabilization if necessary.
Tolerance and the potential for addiction associated with diazepam are significant concerns. Physical and psychological addiction to diazepam is well-documented.
Tolerance to the sedative-hypnotic effects of diazepam develops within a few days of continuous use, and after discontinuation, it typically returns to baseline within 7-14 days. However, in some cases, this process may take considerably longer, commensurate with the duration and intensity of long-term usage.
Abrupt cessation of diazepam use, especially following several weeks or more of consistent dosing, can lead to withdrawal or rebound symptoms, necessitating a gradual dose reduction. It is crucial to taper off benzodiazepines in a controlled manner, as discontinuation can be difficult and potentially life-threatening, with increased risks of hypertension, seizures, and even death. During withdrawal, it’s advisable to avoid drugs that lower the seizure threshold, such as tramadol.
Diazepam induces cross-tolerance with all other benzodiazepines, meaning that its consumption reduces the effectiveness of all benzodiazepines.
Benzodiazepine overdose may occur when taken in excessive amounts or conjunction with other depressants. This becomes particularly dangerous when combined with other GABAergic depressants, including barbiturates and alcohol, as they operate similarly but bind to distinct allosteric sites on the GABAA receptor, intensifying their effects. The result is a higher frequency and longer duration of the ion pore opening on the GABAA receptor. Benzodiazepine overdose constitutes a medical emergency and can lead to a coma, permanent brain damage, or death if not promptly and adequately treated.
Symptoms of benzodiazepine overdose include severe thought deceleration, slurred speech, confusion, delusions, respiratory depression, coma, or death. While flumazenil is sometimes used to treat benzodiazepine overdoses, care primarily involves supportive measures in a hospital setting.
Dangerous interactions should not be underestimated, as combining certain substances can be life-threatening. Below is a list of common potentially dangerous combinations, although it may not cover all scenarios. Independent research is crucial to ensure the safety of combining two or more substances before consumption.
- Depressants (1,4-Butanediol, 2-methyl-2-butanol, alcohol, barbiturates, GHB/GBL, methaqualone, opioids): This combination can result in dangerous levels of respiratory depression, muscle relaxation, sedation, and amnesia, potentially leading to unconsciousness and suffocation. In such cases, users should attempt to lie in the recovery position or have a friend move them into it if vomiting occurs.
- Dissociatives: Combining benzodiazepines with dissociatives increases the risk of vomiting during unconsciousness and the potential for suffocation. As with other combinations, users should attempt to adopt the recovery position if necessary.
- Stimulants: Mixing benzodiazepines with inspirations can lead to excessive intoxication. Stimulants diminish the sedative effects of benzodiazepines, potentially causing heightened disinhibition and other adverse effects once the stimulant’s effects wear off. Hydration should be monitored, as this combination may lead to severe dehydration. Users should strictly limit benzodiazepine dosing when combining these substances.
Legal status
Internationally, diazepam is categorized as a Schedule IV controlled substance by the Convention on Psychotropic Substances. It is subject to regulation as a prescription medication in most countries.
Here are specific regulations in select countries:
- Australia: Diazepam is classified as a Schedule 4 substance in the Poisons Standard, requiring it only to be available by prescription.
- Austria: Diazepam is permitted for medical use under the AMG (Arzneimittelgesetz Österreich) and is illegal to sell or possess without a prescription, as per the SMG (Suchtmittelgesetz Österreich).
- Czech Republic: Diazepam is categorized as a Schedule IV (List 7) substance and is exclusively available with a prescription that does not bear a blue stripe (§ 1, g), as outlined in Nařízení vlády č. 463/2013 Sb.)
- Germany: Diazepam has been regulated under Anlage III BtMG (Narcotics Act, Schedule III) since August 1, 1986. It can only be prescribed using a narcotic prescription form, with exceptions for preparations containing up to 10 mg diazepam per dosage form and solutions with up to 1% diazepam and less than 250 mg diazepam in total per packaging unit.
- Russia: Diazepam has been classified as a Schedule III controlled substance since 2013.
- Switzerland: Diazepam is a controlled substance listed explicitly under Verzeichnis B. Medicinal use is permitted.
- United Kingdom: Diazepam is a controlled drug under Schedule IV, Part I (CD Benz POM) of the Misuse of Drugs Regulations 2001. It can be possessed with a valid prescription. The Misuse of Drugs Act 1971 deems it illegal to have the substance without a prescription, classifying it as a Class C drug for such purposes.
FAQ
1. What is Diazepam?
- Diazepam is a medication that belongs to the benzodiazepine class of drugs. It is commonly prescribed to treat various conditions, including anxiety disorders, muscle spasms, and alcohol withdrawal symptoms. Diazepam works by calming the brain and nerves.
2. How does Diazepam work?
- Diazepam enhances the activity of a neurotransmitter called gamma-aminobutyric acid (GABA) in the brain. GABA is responsible for reducing excessive brain activity, which helps to alleviate anxiety, induce relaxation, and relieve muscle tension.
3. What conditions are typically treated with Diazepam?
- Diazepam is prescribed for anxiety disorders, panic attacks, muscle spasms, seizures, alcohol withdrawal, and as a preoperative sedative. It may also be used in treating certain sleep disorders and as an adjunct to anaesthesia.
4. Is Diazepam safe to use?
- Diazepam is generally safe when used as directed by a healthcare professional. However, it can be habit-forming and should only be used under close medical supervision. It may not suit everyone, and potential risks should be discussed with a healthcare provider.
5. How should I take Diazepam?
- Follow your doctor’s instructions carefully. Diazepam is usually taken orally as a tablets or liquid. The dosage and frequency of administration will vary depending on your condition. Please do not exceed the prescribed dose or use it longer than recommended.
6. What are the potential side effects of Diazepam?
- Common side effects may include drowsiness, dizziness, muscle weakness, and changes in coordination. Serious side effects are rare, including allergic reactions, memory problems, and paradoxical reactions such as increased anxiety or agitation. Contact your healthcare provider if you experience any unusual or severe side effects.
7. Can Diazepam be addictive?
- Yes, Diazepam has the potential for addiction and dependence, mainly when used for extended periods or in higher doses than prescribed. It is essential to use it as directed by your doctor and not to abruptly stop taking it without medical guidance to avoid withdrawal symptoms.
8. Can I drink alcohol while taking Diazepam?
- Combining alcohol with Diazepam can lead to dangerous side effects, including extreme drowsiness, impaired coordination, and memory problems. It is strongly advised to avoid alcohol while taking this medication.
9. How long can I take Diazepam?
- Diazepam is typically prescribed for short-term use, such as a few weeks. A healthcare provider should carefully monitor long-term use due to tolerance, dependence, and withdrawal risks.
10. Is driving or operating heavy machinery safe while taking Diazepam?
- Diazepam can impair coordination and cognitive function, so driving or operating machinery while under its influence is unsafe. Before engaging in such activities, it’s crucial to wait until you know how Diazepam affects you.
11. Can I take Diazepam during pregnancy or while breastfeeding?
- Diazepam should be used during pregnancy or breastfeeding only if the benefits outweigh the risks and under the strict supervision of a healthcare provider. It can potentially harm the developing fetus or pass into breast milk, affecting the baby.
References
- Risks Associated with Combining Depressants – TripSit
- Wick, J. Y. (September 1 2013). “The Evolution of Benzodiazepines”. The Consultant Pharmacist. 28 (9): 538–548. doi:10.4140/TCP.n.2013.538. ISSN 0888-5109.
- Calcaterra, N. E., Barrow, J. C. (April 16 2014). “Classics in Chemical Neuroscience: Diazepam (Valium)”. ACS Chemical Neuroscience. 5 (4): 253–260. doi:10.1021/cn5000056. ISSN 1948-7193.
- WHO Model List (2005) | WHO Model List
- Mandrioli, R., Mercolini, L., Raggi, M. A. (October 2008). “Benzodiazepine Metabolism: An Analytical Perspective”. Current Drug Metabolism. 9 (8): 827–844. doi:10.2174/138920008786049258. ISSN 1389-2002.
- Lann, M. A., Molina, D. K. (June 2009). “A Fatal Case of Benzodiazepine Withdrawal”. The American Journal of Forensic Medicine and Pathology. 30 (2): 177–179. doi:10.1097/PAF.0b013e3181875aa0. ISSN 1533-404X.
- Kahan, M., Wilson, L., Mailis-Gagnon, A., Srivastava, A. (November 2011). “Canadian Guidelines for Safe and Effective Use of Opioids for Chronic Noncancer Pain. Appendix B-6: Benzodiazepine Tapering”. Canadian Family Physician. 57 (11): 1269–1276. ISSN 0008-350X.
- Unseld, E.; Krishna, D. R.; Fischer, C.; Klotz, U. (1989). “Detection of Desmethyldiazepam and Diazepam in the Brain of Different Species and Plants”. Biochemical Pharmacology. 38 (15): 2473–2478. doi:10.1016/0006-2952(89)90091-9. eISSN 1873-2968. ISSN 0006-2952.
- Sample, I. (2005), Leo Sternbach, retrieved July 8 2019
- Barondes, S. H. (2003). Advancements in Psychiatric Medications: Beyond Prozac. Oxford University Press. ISBN 9780195151305.
- Marshall, K. P., Georgievskava, Z., Georgievsky, I. (June 2009). “Social Reactions to Valium and Prozac: A Cultural Lag Perspective of Drug Diffusion and Adoption”. Research in Social and Administrative Pharmacy. 5 (2): 94–107. doi:10.1016/j.sapharm.2008.06.005. ISSN 1551-7411.
- Mariani, M. (2015), Poison Pill – How the American Opiate Epidemic Began with a Single Pharmaceutical Company, retrieved January 10 2018
- Mikota SK, Plumb DC (2005). “Diazepam”. The Elephant Formulary. Elephant Care International. Archived from the original on 8 September 2005.
- Taft, W. C., DeLorenzo, R. J. (May 1984). “Micromolar-Affinity Benzodiazepine Receptors Regulate Voltage-Sensitive Calcium Channels in Nerve Terminal Preparations”. Proceedings of the National Academy of Sciences. 81 (10): 3118–3122. doi:10.1073/pnas.81.10.3118. ISSN 0027-8424.
- “COMMUNICATIONS”. British Journal of Pharmacology. 84 (1): 1P–77P. January 1985. doi:10.1111/j.1476-5381.1985.tb17368.x. ISSN 0007-1188.
- “National Highway Traffic Safety Administration Drugs and Human Performance Fact Sheet – Diazepam”. Archived from the original on March 27 2017.
- Tan, K. R., Rudolph, U., Lüscher, C. (April 2011). “Hooked on Benzodiazepines: GABAA Receptor Subtypes and Addiction”. Trends in Neurosciences. 34 (4): 188–197. doi:10.1016/j.tins.2011.01.004. ISSN 0166-2236.
- Whirl-Carrillo, M., McDonagh, E. M., Hebert, J. M., Gong, L., Sangkuhl, K., Thorn, C. F., Altman, R. B., Klein, T. E. (October 2012). “Pharmacogenomics Knowledge for Personalized Medicine”. Clinical Pharmacology & Therapeutics. 92 (4): 414–417. doi:10.1038/clpt.2012.96. ISSN 0009-9236.
- Zakusov, V. V., Ostrovskaya, R. U., Kozhechkin, S. N., Markovich, V. V., Molodavkin, G. M., Voronina, T. A. (October 1977). “Further Evidence for GABAergic Mechanisms in the Action of Benzodiazepines”. Archives Internationales De Pharmacodynamie Et De Therapie. 229 (2): 313–326. ISSN 0003-9780.
- Haefely, W. (June 29 1984). “Benzodiazepine Interactions with GABA Receptors”. Neuroscience Letters. 47 (3): 201–206. doi:10.1016/0304-3940(84)90514-7. ISSN 0304-3940.
- McLean, M. J., Macdonald, R. L. (February 1988). “Benzodiazepines, but Not Beta Carbolines, Limit High-Frequency Repetitive Firing of Action Potentials of Spinal Cord Neurons in Cell Culture”. The Journal of Pharmacology and Experimental Therapeutics. 244 (2): 789–795. ISSN 0022-3565.
- Saïas, T., Gallarda, T. (September 2008). “[Paradoxical Aggressive Reactions to Benzodiazepine Use: A Review]”. L’Encephale. 34 (4): 330–336. doi:10.1016/j.encep.2007.05.005. ISSN 0013-7006.
- Paton, C. (December 2002). “Benzodiazepines and Disinhibition: A Review”. Psychiatric Bulletin. 26 (12): 460–462. doi:10.1192/pb.26.12.460. ISSN 0955-6036.
- Bond, A. J. (January 1 1998). “Drug-Induced Behavioral Disinhibition”. CNS Drugs. 9 (1): 41–57. doi:10.2165/00023210-199809010-00005. ISSN 1179-1934.
- Drummer, O. H. (February 2002). “Benzodiazepines – Effects on Human Performance and Behavior”. Forensic Science Review. 14 (1–2): 1–14. ISSN 1042-7201.
- Goyal, S. (March 14 1970). “Drugs and Dreams”. Canadian Medical Association Journal. 102 (5): 524. ISSN 0008-4409.
- Nutt, D., King, L. A., Saulsbury, W., Blakemore, C. (March 24 2007). “Development of a Rational Scale to Assess the Harm of Drugs of Potential Misuse”. The Lancet. 369 (9566): 1047–1053. doi:10.1016/S0140-6736(07)60464-4. ISSN 0140-6736.
- Drugs.com – Diazepam
- Greenblatt, D. J., Woo, E., Allen, M. D., Orsulak, P. J., Shader, R. I. (20 October 1978). “Rapid Recovery from Massive Diazepam Overdose”. JAMA. 240 (17): 1872–1874. ISSN 0098-7484.
- Diazepam (PIM 181)
- Diazepam (Diazepam Injection): Uses, Dosage, Side Effects, Interactions, Warning
- Janicak, P. G., Marder, S. R., Pavuluri, M. N. (October 25 2010). Principles and Practice of Psychopharmacotherapy. Lippincott Williams & Wilkins. ISBN 9781605475653.
- Verster, J. C., Volkerts, E. R. (7 June 2006). “Clinical Pharmacology, Clinical Efficacy, and Behavioral Toxicity of Alprazolam: A Review of the Literature”. CNS Drug Reviews. 10 (1): 45–76. doi:10.1111/j.1527-3458.2004.tb00003.x. ISSN 1080-563X.
- Galanter, M., Kleber, H. D. (2008). Advances in Substance Abuse Treatment. American Psychiatric Pub. ISBN 9781585622764.
- Twyman, R. E., Rogers, C. J., Macdonald, R. L. (March 1989). “Differential Regulation of Gamma-Aminobutyric Acid Receptor Channels by Diazepam and Phenobarbital”. Annals of Neurology. 25 (3): 213–220. doi:10.1002/ana.410250302. ISSN 0364-5134.
- Hoffman, E. J., Warren, E. W. (September 1993). “Flumazenil: A Benzodiazepine Antagonist”. Clinical Pharmacy. 12 (9): 641–656; quiz 699–701. ISSN 0278-2677.
- International Narcotics Control Board (2003) | INCB Report
- “Poisons Standard December 2019”. Office of Parliamentary Counsel. November 14, 2019. Retrieved December 28, 2019.
- European Union Legislation
- Czech Republic Legislation
- “Zweite Verordnung zur Änderung betäubungsmittelrechtlicher Vorschriften” (PDF). Bundesgesetzblatt Jahrgang 1986 Teil I (in German). Bundesanzeiger Verlag. July 29, 1986. Retrieved December 26, 2019.
- “Anlage III BtMG” (in German). Bundesministerium der Justiz und für Verbraucherschutz. Retrieved December 26, 2019.
- Постановление Правительства РФ от 04.02.2013 N 78 “О внесении изменений в некоторые акты Правительства Российской Федерации” – КонсультантПлюс9
- “Verordnung des EDI über die Verzeichnisse der Betäubungsmittel, psychotropen Stoffe, Vorläuferstoffe und Hilfschemikalien” (in German). Bundeskanzlei [Federal Chancellery of Switzerland]. Retrieved January 1, 2020.
- [Drugs Licensing](insert the relevant link)
Leave a Reply