Contents
Summary
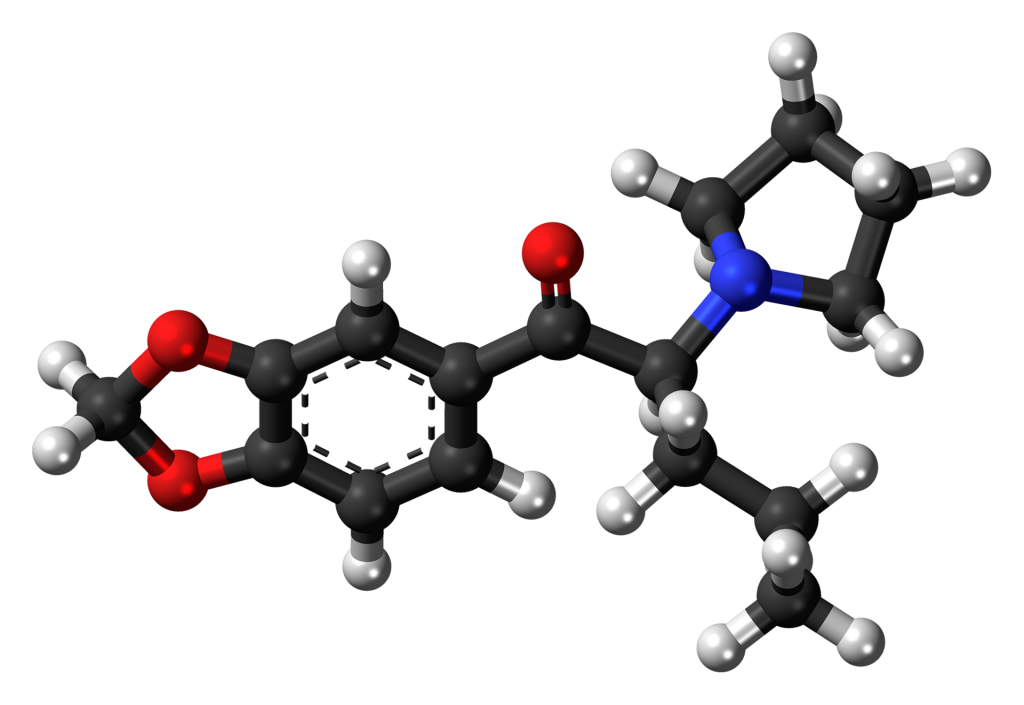
Methylenedioxypyrovalerone (MDPV) is a cathinone-class stimulant that functions as a norepinephrine-dopamine reuptake inhibitor (NDRI). It originated in the 1960s through development by a team at Boehringer Ingelheim. Notably, MDPV exhibits considerably stronger activity at the dopamine transporter compared to the norepinephrine transporter, while showing minimal activity at the serotonin transporter. MDPV remained relatively obscure as a stimulant until around 2004 when reports emerged of its availability as a designer drug. In the United States, products containing MDPV were sold with labels indicating “bath salts” and marketed as recreational substances in gas stations, a practice reminiscent of the marketing for products like Spice and K2 as incense. The sale of MDPV as “bath salts” ceased in 2011 following a ban.
| Identifiers | |
|---|---|
| IUPAC name | |
| CAS Number | 687603-66-3 24622-62-6 (HCl) |
|---|---|
| PubChem CID | 20111961 |
| ChemSpider | 16788110 |
| UNII | E7LD6JMR0L |
| CompTox Dashboard (EPA) | DTXSID90897461 |
| Chemical and physical data | |
| Formula | C16H21NO3 |
| Molar mass | 275.343 g/mol (freebase) g·mol−1 |
Appearance
The hydrochloride salt of MDPV presents as an exceptionally fine crystalline powder that is hygroscopic, tending to clump, reminiscent of powdered sugar. Its color varies from pure white to yellowish-tan, and it carries a subtle odor that intensifies as it changes color. Impurities likely include pyrrolidine or alpha-dibrominated alkylphenones, arising from excess pyrrolidine or incomplete amination during synthesis. These impurities contribute to its discoloration and can emit a fishy (pyrrolidine) or bromine-like odor, particularly upon exposure to air, moisture, or bases.
Pharmacology
MDPV lacks FDA-approved medical applications. It has demonstrated robust reinforcing effects and compulsive self-administration in rats, findings that were provisionally established based on documented cases of misuse and addiction in humans before animal testing was conducted. MDPV is the 3,4-methylenedioxy ring-substituted analog of pyrovalerone, a compound developed in the 1960s that was initially used for chronic fatigue treatment and as an anorectic agent but raised concerns due to issues of abuse and dependence[10]. Other drugs sharing a similar chemical structure include α-pyrrolidinopropiophenone (α-PPP), 4′-methyl-α-pyrrolidinopropiophenone (M-α-PPP), 3′,4′-methylenedioxy-α-pyrrolidinopropiophenone (MDPPP), and 1-phenyl-2-(1-pyrrolidinyl)-1-pentanone (α-PVP).
Effects
MDPV functions as a stimulant and has been reported to induce effects similar to those of cocaine, methylphenidate, and amphetamines. Its primary psychological effects are approximately 3 to 4 hours, followed by aftereffects, such as tachycardia, hypertension, and mild stimulation, lasting 6 to 8 hours. High doses have been known to cause intense, prolonged panic attacks in individuals intolerant to stimulants, and there are anecdotal accounts of psychosis resulting from sleep deprivation and addiction when using higher doses or more frequent intervals. Additionally, it has been repeatedly noted to trigger irresistible cravings for re-administration. Reported modes of intake encompass oral consumption, insufflation, smoking, rectal and intravenous use, with an active range of 3–5 mg and typical doses falling within the 5–20 mg range. In mice, repeated MDPV exposure has been found to induce anxiogenic effects and increase aggressive behavior. Similar observations have been noted in humans. MDPV-treated mice also adapted faster to repeated social isolation, akin to MDMA. A cross-sensitization between MDPV and cocaine has been observed, and both drugs restore drug-seeking behavior concerning each other. Memories associated with MDPV require a longer time to be extinguished. In MDPV-treated mice, a priming dose of cocaine induces notable neuroplasticity, indicating a heightened vulnerability to cocaine abuse.
Long-term Effects
The long-term effects of MDPV on humans have not been extensively studied. However, research has suggested that mice treated with MDPV during adolescence exhibit reinforcing behavior patterns towards cocaine that surpass control groups. These behavioral changes are associated with alterations in factor expression directly linked to addiction, indicating an increased susceptibility to cocaine abuse.
Metabolism
MDPV undergoes phase 1 metabolism in the liver through CYP450 2D6, 2C19, 1A2, and COMT. This process transforms it into methyl catechol and pyrrolidine, which are further glucuronate, enabling excretion via the kidneys. Only a small fraction of metabolites is excreted in the stools. Notably, free pyrrolidine is not detectable in the urine.
Detection in Biological Specimens
MDPV can be quantified in blood, plasma, or urine through gas chromatography-mass or liquid chromatography-mass spectrometry. This is used to confirm a diagnosis of poisoning in hospitalized patients or to provide evidence in medicolegal death investigations. Blood or plasma MDPV concentrations typically range from 10–50 μg/L in recreational users, exceeding 50 μg/L in intoxicated patients, and exceeding 300 μg/L in cases of acute overdose.
Legality
In the UK, MDPV is classified as a Class B drug under The Misuse of Drugs Act 1971 (Amendment) Order 2010, rendering it illegal to sell, buy, or possess without a license. MDPV is explicitly listed as a controlled substance in Finland (listed in Appendix IV substance as of June 28, 2010), Denmark, and Sweden. In Western Australia, MDPV was included in Appendix A Schedule 9 of the Poisons Act 1964 as of February 11, 2012, and carries severe penalties for sale or possession. Canada placed MDPV on Schedule I of the Controlled Drugs and Substances Act on September 26, 2012. In the United States, MDPV is a DEA federally scheduled drug temporarily banned by the DEA on October 21, 2011. Several states and regions in the U.S. have specific laws regarding MDPV, including bans in Louisiana, Florida, Kentucky, New Jersey, Tennessee, and Maine.
Documented Fatalities
Numerous documented fatalities and non-fatal intoxications associated with MDPV use have been reported between September 2009 and August 2013 in various European countries.
Overdose Treatment
In cases of MDPV overdose, physicians often administer anxiolytics like benzodiazepines to reduce drug-induced activity in the brain and body. In severe cases, general anesthesia has been utilized due to the ineffectiveness of sedatives. Treatment for severe hypertension, tachycardia, agitation, or seizures in emergency departments typically involves large doses of lorazepam administered intravenously or intramuscularly. Haloperidol is an alternative treatment if lorazepam is ineffective. Beta-blockers are not recommended as they can lead to paradoxical rises in blood pressure. Electroconvulsive therapy (ECT) has been found to improve persistent psychotic symptoms linked to repeated MDPV use.
FAQ
- What is Methylenedioxypyrovalerone (MDPV)?
- MDPV is a synthetic stimulant of the cathinone class. Initially developed in the 1960s, it acts as a norepinephrine-dopamine reuptake inhibitor (NDRI).
- What are the effects of MDPV?
- MDPV acts as a stimulant and produces effects similar to cocaine, methylphenidate, and amphetamines. These effects typically last for about 3 to 4 hours, with aftereffects like increased heart rate, high blood pressure, and mild stimulation that can persist for 6 to 8 hours. Higher doses can lead to intense panic attacks and potential psychosis.
- Is MDPV legal?
- The legal status of MDPV varies by country and region. In some places, it is classified as a controlled substance and is illegal to sell, buy, or possess without a license. It was temporarily banned in the United States in 2011.
- What are the long-term effects of MDPV use?
- The long-term effects of MDPV on humans have not been extensively studied. However, research in mice suggests that MDPV use during adolescence may increase vulnerability to cocaine abuse.
- How is MDPV metabolized in the body?
- MDPV undergoes liver metabolism via various enzymes, including CYP450 2D6, 2C19, 1A2, and COMT. It is then excreted primarily through the kidneys, with only a small fraction of metabolites in the stools.
- Is there treatment for MDPV overdose?
- In cases of MDPV overdose, medical professionals typically use anxiolytics like benzodiazepines to reduce drug-induced activity in the brain and body. Severe cases may require general anesthesia. Treatment for severe hypertension, tachycardia, agitation, or seizures often involves large doses of lorazepam or haloperidol.
- Are there documented fatalities associated with MDPV use?
- There have been documented fatalities and non-fatal intoxications related to MDPV use. In some cases, MDPV was found in the systems of individuals who experienced adverse health effects.
- Can MDPV be detected in biological specimens?
- MDPV can be quantified in blood, plasma, or urine through various laboratory techniques, such as gas chromatography-mass or liquid chromatography-mass spectrometry. This is done to confirm diagnoses of poisoning or for medicolegal investigations.
- Is MDPV similar to other drugs?
- MDPV shares similarities with other substances, including pyrovalerone and related cathinones. It is chemically related to α-pyrrolidinopropiophenone (α-PPP), 4′-methyl-α-pyrrolidinopropiophenone (M-α-PPP), 3′,4′-methylenedioxy-α-pyrrolidinopropiophenone (MDPPP), and 1-phenyl-2-(1-pyrrolidinyl)-1-pentanone (α-PVP).
References
1. EMCDDA–Europol Joint Report on a New Psychoactive Substance: MDPV (3,4-Methylenedioxypyrovalerone) (PDF). European Monitoring Centre for Drugs and Drug Addiction (EMCDDA). January 2014. Retrieved June 27, 2016. [Archived PDF from the original on August 15, 2016]
2. Baumann MH, Partilla JS, Lehner KR, Thorndike EB, Hoffman AF, Holy M, et al. (March 2013). “Powerful cocaine-like actions of 3,4-methylenedioxypyrovalerone (MDPV), a principal constituent of psychoactive ‘bath salts’ products”. Neuropsychopharmacology. 38 (4): 552–62. doi:10.1038/npp.2012.204. PMID 23072836. [PMC 3572453]
3. Simmler LD, Buser TA, Donzelli M, Schramm Y, Dieu LH, Huwyler J, et al. (January 2013). “Pharmacological characterization of designer cathinones in vitro”. British Journal of Pharmacology. 168 (2): 458–70. doi:10.1111/j.1476-5381.2012.02145.x. PMID 22897747. [PMC 3572571]
4. US 3478050, Koppe H, Ludwig G, Zeile K, “1-(3′,4′-methylenedioxy-phenyl)-2-pyrrolidino-alkanones-(1)”, issued November 1969, assigned to CH Boehringer Sohn AG and Co and KG Boehringer Ingelheim GmbH.
5. Slomski A (December 2012). “A Trip on ‘Bath Salts’ is Cheaper than Meth or Cocaine but Much More Dangerous”. JAMA. 308 (23): 2445–7. doi:10.1001/jama.2012.34423. PMID 23288310.
6. Brandt SD, Freeman S, Sumnall HR, Measham F, Cole J (September 2011). “Analysis of NRG ‘Legal Highs’ in the UK: Identification and Formation of Novel Cathinones”. Drug Testing and Analysis. 3 (9): 569–75. doi:10.1002/dta.204. PMID 21960541. [CiteSeerX 10.1.1.687.9467]
7. Westphal F, Junge T, Rösner P, Sönnichsen F, Schuster F (September 2009). “Mass and NMR Spectroscopic Characterization of 3,4-Methylenedioxypyrovalerone: A Designer Drug with Alpha-Pyrrolidinophenone Structure”. Forensic Science International. 190 (1–3): 1–8. doi:10.1016/j.forsciint.2009.05.001. PMID 19500924.
8. Watterson LR, Kufahl PR, Nemirovsky NE, Sewalia K, Grabenauer M, Thomas BF, et al. (March 2014). “Potent Rewarding and Reinforcing Effects of the Synthetic Cathinone 3,4-Methylenedioxypyrovalerone (MDPV)”. Addiction Biology. 19 (2): 165–74. doi:10.1111/j.1369-1600.2012.00474.x. PMID 22784198. [PMC 3473160]
9. Coppola M, Mondola R (January 2012). “3,4-Methylenedioxypyrovalerone (MDPV): Chemistry, Pharmacology, and Toxicology of a New Designer Drug of Abuse Marketed Online”. Toxicology Letters. 208 (1): 12–5. doi:10.1016/j.toxlet.2011.10.002. PMID 22008731.
10. Seeger E (October 1964). “US Patent 3314970 – α-Pyrrolidino Ketones”. Boehringer Ingelheim. Retrieved June 27, 2016. [Archived from the original on June 19, 2015]
11. “Report on MDPV” (PDF). Drugs of Concern. DEA. May 2013. Retrieved June 27, 2016. [Archived PDF from the original on June 11, 2016]
12. “Consideration of the Cathinones” (PDF). Advisory Council on the Misuse of Drugs. March 31, 2010. Retrieved June 27, 2016. [Archived PDF from the original on September 16, 2016]
13. Duart-Castells L, López-Arnau R, Buenrostro-Jáuregui M, Muñoz-Villegas P, Valverde O, Camarasa J, et al. (January 2019). “Neuroadaptive Changes and Behavioral Effects After a Sensitization Regime of MDPV”. Neuropharmacology. 144: 271–281. doi:10.1016/j.neuropharm.2018.10.005. PMID 30321610. [hdl:2445/148191]
14. Duart-Castells L, López-Arnau R, Vizcaíno S, Camarasa J, Pubill D, Escubedo E (May 2019). “7,8-Dihydroxyflavone Blocks the Development of Behavioral Sensitization to MDPV, but Not to Cocaine: Differential Role of the BDNF-TrkB Pathway”. Biochemical Pharmacology. 163: 84–93. doi:10.1016/j.bcp.2019.02.004. PMID 30738029. [hdl:2445/130480]
15. Duart-Castells L, Blanco-Gandía MC, Ferrer-Pérez C, Puster B, Pubill D, Miñarro J, et al. (June 2020). “Cross-Reinstatement Between 3,4-Methylenedioxypyrovalerone (MDPV) and Cocaine Using Conditioned Place Preference”. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 100: 109876. doi:10.1016/j.pnpbp.2020.109876. PMID 31991149. [S2CID 210896469]
16. López-Arnau R, Luján MA, Duart-Castells L, Pubill D, Camarasa J, Valverde O, Escubedo E (May 2017). “Exposure of Adolescent Mice to 3,4-Methylenedioxypyrovalerone Increases the Psychostimulant, Rewarding, and Reinforcing Effects of Cocaine in Adulthood”. British Journal of Pharmacology. 174 (10): 1161–1173. doi:10.1111/bph.13771. PMID 28262947. [PMC 5406300]
17. Kalapos MP (December 2011). “[3,4-Methylene-Dioxy-Pyrovalerone (MDPV) Epidemic?]”. Orvosi Hetilap. 152 (50): 2010–9. PMID 22112374.
18. Strano-Rossi S, Cadwallader AB, de la Torre X, Botrè F (September 2010). “Toxicological Determination and In Vitro Metabolism of the Designer Drug Methylenedioxypyrovalerone (MDPV) by Gas Chromatography/Mass Spectrometry and Liquid Chromatography/Quadrupole Time-of-Flight Mass Spectrometry”. Rapid Communications in Mass Spectrometry. 24 (18): 2706–14. doi:10.1002/rcm.4692. PMID 20814976.
19. Michaelis W, Russel JH, Schindler O (May 1970). “The Metabolism of Pyrovalerone Hydrochloride”. Journal of Medicinal Chemistry. 13 (3): 497–503. doi:10.1021/jm00297a036. PMID 5441133.
20. Meyer MR, Du P, Schuster F, Maurer HH (December 2010). “Studies on the Metabolism of the α-Pyrrolidinophenone Designer Drug Methylenedioxy-Pyrovalerone (MDPV) in Rat and Human Urine and Human Liver Microsomes Using GC-MS and LC-High-Resolution MS and Its Detectability in Urine by GC-MS”. Journal of Mass Spectrometry. 45 (12): 1426–42. doi:10.1002/jms.1859. PMID 21053377.
21. Baselt RC (2014). Disposition of Toxic Drugs and Chemicals in Man. Seal Beach, CA: Biomedical Publications. pp. 1321–1322. ISBN 978-0-9626523-9-4.
22. “A Change to the Misuse of Drugs Act 1971: Control of Mephedrone and Other Cathinone Derivatives”. Home Office. April 16, 2010. [Archived from the original on January 25, 2013]
23. “The Misuse of Drugs Act 1971 (Amendment) Order 2010”. Home Office. April 12, 2010. [Archived from the original on May 22, 2013. Retrieved November 19, 2012]
24. Naantalissa A (June 28, 2010). “Finlex: Huumausaineina Pidettävistä Aineista, Valmisteista ja Kasveista Annetun Valtioneuvoston Asetuksen Liitteen IV Muuttamisesta”. Oikeusministeriö (in Finnish). [Archived from the original on July 20, 2011. Retrieved January 25, 2011]
25. “Hovrätten Skärper Straff I MDPV-Dom”. Norrköpings Tidningar (in Swedish). June 4, 2010. [Archived from the original on March 13, 2016. Retrieved June 27, 2016]
26. “Emerging Drug, MDPV Banned in WA”. Government of Western Australia. February 8, 2012. [Archived from the original on August 15, 2016. Retrieved June 27, 2016]
27. “‘Bath Salts’ Drug Ingredient Banned in Canada”. CBC News. September 26, 2012. [Archived from the original on August 11, 2016. Retrieved June 27, 2016]
28. “Chemicals Used in ‘Bath Salts’ Now Under Federal Control and Regulation” (Press release). Drug Enforcement Administration (DEA). October 21, 2011. [Archived from the original on August 15, 2016. Retrieved June 27, 2016]
29. Allen G (February 8, 2011). “Florida Bans Cocaine-Like ‘Bath Salts’ Sold in Stores”. NPR. [Archived from the original on February 14, 2019. Retrieved April 2, 2018]
30. Beshear S (March 23, 2011). “Gov. Beshear Signs Law Banning New Synthetic Drugs” (Press release). Commonwealth of Kentucky. [Archived from the original on May 13, 2016. Retrieved June 27, 2016]
31. Rowe A (September 2, 2011). “Governor Bans Bath Salts After Student’s Death”. Daily Targum. [Archived from the original on August 12, 2016. Retrieved June 27, 2016]
32. Giambusso D (September 2, 2011). “Cranford Man Charged with Murdering Girlfriend; Toxicology Report Shows No Trace of ‘Bath Salts'”. NJ.com. [Archived from the original on March 9, 2014. Retrieved January 27, 2014]
33. “State of Tennessee Public Chapter No. 169 House Bill No. 457” (PDF). State of Tennessee. April 18, 2011. [Archived PDF from the original on January 20, 2017. Retrieved June 27, 2016]
34. “New Law Sets Fine at $350 for ‘Bath Salts’ Possession”. Portland Press Herald. July 7, 2011. [Archived from the original on August 16, 2016. Retrieved June 27, 2016]
35. “Ohio Amendment to Controlled Substances Act HB 64”. Ohio General Assembly Archives. October 17, 2011. [Archived from the original on June 30, 2015. Retrieved January 11, 2015]
36. Kreider R (December 8, 2011). “House Votes to Ban ‘Spice,’ ‘Bath Salts'”. ABC News. [Archived from the original on May 2, 2020. Retrieved June 28, 2020]
37. Wilson T (May 12, 2011). “Illinois Lawmakers Target Bath Salts Used as a Drug”. Chicago Tribune. [Archived from the original on August 12, 2016. Retrieved June 27, 2016]
38. “Emergency Department Visits After Use of a Drug Sold as ‘Bath Salts’ — Michigan, November 13, 2010 – March 31, 2011”. Morbidity and Mortality Weekly Report. Vol. 60, no. 19. Centers for Disease Control and Prevention (CDC). May 2011. [Archived from the original on September 7, 2017. Retrieved September 10, 2017]
39. Boshuisen K, Arends JE, Rutgers DR, Frijns CJ (May 2012). “A Young Man with Hemiplegia After Inhaling the Bath Salt ‘Ivory Wave'”. Neurology. 78 (19): 1533–4. doi:10.1212/WNL.0b013e3182553c70. PMID 22539576.
40. Salter J, Jim S (April 6, 2011). “Synthetic Drugs Sent Thousands to ER”. NBC News. [Archived from the original on July 16, 2016. Retrieved June 27, 2016]
41. Goodnough A, Zezima K (July 16, 2011). “An Alarming New Stimulant, Legal in Many States”. New York Times. [Archived from the original on April 15, 2021. Retrieved February 27, 2017]
42. “‘Bath Salts’ Health Care Provider Fact Sheet” (PDF). Michigan Department of Community Health. April 30, 2012. [Archived PDF from the original on May 1, 2017. Retrieved June 27, 2016]
43. Penders TM, Gestring RE, Vilensky DA (November 2012). “Intoxication Delirium Following Use of Synthetic Cathinone Derivatives”. The American Journal of Drug and Alcohol Abuse. 38 (6): 616–7. doi:10.3109/00952990.2012.694535. PMID 22783894. [S2CID 207428569]
44. Penders TM, et al. (December 2013). “Electroconvulsive Therapy Improves Persistent Psychosis After Repeated Use of Methylenedioxypyrovalerone (‘Bath Salts’)”. The Journal of ECT. 29 (4): 59–60. doi:10.1097/YCT.0b013e3182887bc2. PMID 23609518. [S2CID 45842375].