Contents
Summary
Dihydrocodeine, a semi-synthetic morphinan opioid analgesic, is prescribed to alleviate pain or serve as an antitussive agent, either in isolation or in combination with paracetamol or aspirin. This pharmaceutical compound originated in Germany in 1908 and entered the market for medical use in 1911.
Various names, including Drocode, Paracodeine, and Parzone, recognize Dihydrocodeine. It boasts an array of brand names such as Synalgos DC, Panlor DC, Panlor SS, Contugesic, Bron Tablet, New Bron Solution-ACE, Pabron S Gold W Tablets, Huscode, Drocode, Paracodin, Codidol, Dehace, Didor Continus, Dicogesic, Codhydrine, Dekacodin, DHC, DH-Codeine, Didrate, Dihydrin, Hydrocodin, Makatussin, Nadine, Novicodin, Rapacodin, Paramol, Remedeine, Dico, and DF-118.
Dihydrocodeine is accessible in various oral formats, such as tablets, solutions, elixirs, and more. In select regions, it is also offered as an injectable solution for deep subcutaneous and intra-muscular use. It is essential to note that, similar to codeine, intravenous administration should be avoided due to the risk of anaphylaxis and dangerous pulmonary oedema. Additionally, Dihydrocodeine can be obtained in suppository form with a prescription.
As an alternative or complement to codeine, Dihydrocodeine shares a similar chemical structure and is considered to possess analgesic effects that are potentially twice as potent as those of codeine. It is worth highlighting that Dihydrocodeine lacks a ceiling effect, which sets it apart from codeine. Unlike codeine, which is associated with a ceiling effect (typically around 200-600mg/day), Dihydrocodeine allows for the possibility of increased euphoria with higher doses, owing to the absence of this limitation.
| Identifiers | |
|---|---|
| IUPAC name | |
| CAS Number | 125-28-0 |
|---|---|
| PubChem CID | 5284543 |
| IUPHAR/BPS | 7594 |
| DrugBank | DB01551 |
| ChemSpider | 4447600 |
| UNII | N9I9HDB855 |
| KEGG | D07831 |
| ChEMBL | ChEMBL1595 |
| CompTox Dashboard (EPA) | DTXSID5022936 |
| ECHA InfoCard | 100.004.303 |
| Chemical and physical data | |
| Formula | C18H23NO3 |
| Molar mass | 301.386 g·mol−1 |
Chemistry
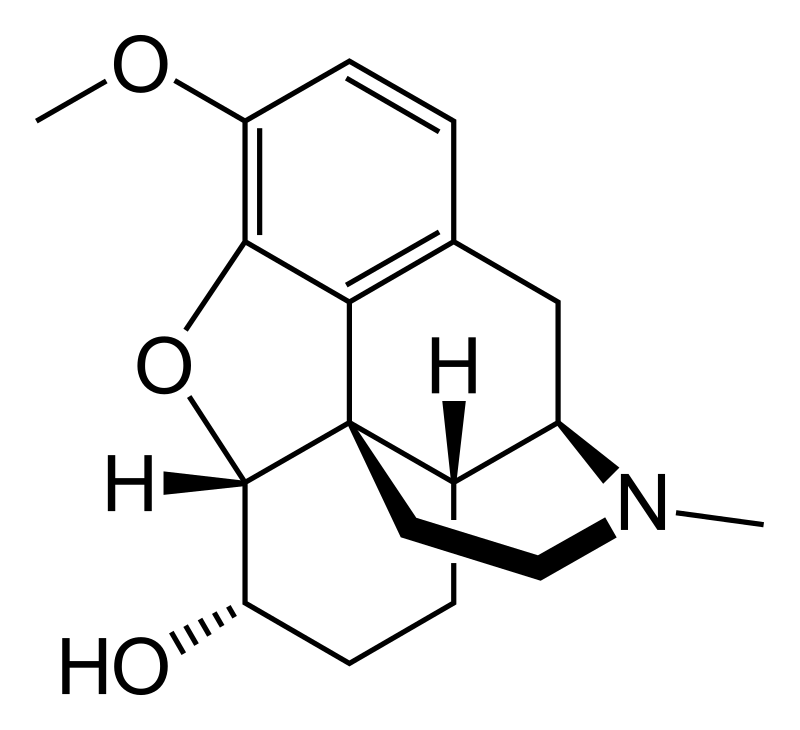
Dihydrocodeine, scientifically known as 4,5-alpha-epoxy-3-methoxy-17-methylmorphinan-6-ol, belongs to the morphinan class of opioids. Within this class, Dihydrocodeine and similar molecules exhibit a complex molecular structure composed of three interconnected benzene rings, forming a zig-zag pattern referred to as phenanthrene. Additionally, a fourth ring containing nitrogen is fused to the phenanthrene at positions R9 and R13, with the nitrogen atom located at R17 within this composite structure. This distinctive arrangement is termed a “morphinan.”
Dihydrocodeine, in common with other morphinans, features an ether bridge connecting two of its rings, specifically binding R4 and R5 through an oxygen moiety. It also includes a hydroxy group (OH-) attached to R6 and a methyl group situated on the nitrogen atom at R17. Notably, in the same ring harbouring the hydroxy group, codeine displays a double bond that is absent in Dihydrocodeine. This disparity contributes to a significantly more stable chemical structure for Dihydrocodeine and profoundly influences its metabolic properties.
The synthesis of Dihydrocodeine from morphine involves the reduction of the 7,8-double bond. This process readily yields dihydromorphine with an efficiency exceeding 95%, which can subsequently undergo methylation to yield Dihydrocodeine. Dihydrocodeine shares structural similarities with other morphinans, including codeine, heroin, ethylmorphine, hydrocodone, and oxycodone.
Pharmacology
Dihydrocodeine exerts its effects by engaging and activating the μ-opioid receptor. This mechanism arises from the structural resemblance of opioids to endogenous endorphins, which occur naturally in the body and also influence the μ-opioid receptor system. The manner in which opioids structurally imitate these innate endorphins leads to the experience of euphoria, pain alleviation, and anxiolytic (anxiety-reducing) effects. This similarity is rooted in the fact that endorphins play a crucial role in diminishing pain, inducing drowsiness, and eliciting sensations of pleasure. Endorphins can be released in response to various stimuli such as pain, vigorous physical activity, orgasm, or heightened emotional excitement.
Dihydrocodeine undergoes metabolic conversion via the CYP2D6 enzyme, resulting in the formation of its active metabolite, dihydromorphine, which possesses potency levels akin to morphine. Additional metabolites with relatively lower activity include dihydrocodeine (produced through CYP3A4) and dihydrocodeine-6-glucuronide. Although dihydrocodeine does yield exceedingly active metabolites like dihydromorphine and dihydromorphine-6-glucuronide, these metabolites are generated in such minuscule quantities that they do not exert clinically significant effects.
Binding affinities (Ki):
- Mu opioid agonist: 325 nM
- Kappa opioid agonist: 14,242 nM
- Delta opioid agonist: 5,905 nM
While dihydrocodeine itself exhibits limited binding to opioid receptors, its principal active metabolite, dihydromorphine, and one of its metabolites, dihydromorphine-6-O-glucuronide, display notably stronger agonistic effects.
Subjective effects
Disclaimer: The following effects are based on anecdotal user reports and personal analyses from contributors to the Subjective Effect Index (SEI) in the open research literature. As a result, they should be approached with a healthy degree of scepticism.
It’s important to note that these effects may not necessarily occur predictably or consistently, although higher doses are more likely to bring about the full range of effects. Moreover, as doses increase, the likelihood of adverse effects, including addiction, severe harm, or even death ☠, becomes more significant.
Physical:
- Compared to codeine, this compound is generally considered to be significantly more euphoric with less itchiness.
- Pain relief
- Itchiness: This effect is less intense when compared to codeine.
- Euphoria: While this substance may be less physically euphoric than morphine or heroin due to metabolic limits on conversion to its active form, it may be considered more euphoric than codeine because of its potent analgesic effects. Euphoria can be described as an intense sensation of physical comfort, warmth, and bliss that spreads throughout the body.
- Respiratory depression: At low to moderate doses, this effect results in a mild to moderate slowing of breath without noticeable impairment. At high doses and overdoses, opioid-induced respiratory depression can lead to shortness of breath, abnormal breathing patterns, semi-consciousness, or unconsciousness. Severe overdoses can result in a coma or death without immediate medical attention.
- Sedation: At higher doses, this compound can induce sedation and is notably more sedating than oxycodone and hydrocodone.
- Constipation
- Cough suppression
- Difficulty urinating
- Pupil constriction
- Decreased libido
- Appetite suppression
- Orgasm suppression
Cognitive:
- The typical cognitive state induced by dihydrocodeine is described as one of intense euphoria, relaxation, anxiety suppression, and pain relief.
- Euphoria: The cognitive euphoria produced by this substance may be less intense than that of morphine or diacetylmorphine (heroin) due to metabolic limits on conversion to its active form. However, it is still capable of extreme intensity and can be overwhelming at higher doses with low tolerance. Powerful and overwhelming feelings of emotional bliss, contentment, and happiness characterize this sensation.
- Anxiety suppression
- Compulsive redosing
- Dream potentiation
Visual:
- Suppressions
- Double vision: At high doses, the eyes may unfocus and refocus uncontrollably, creating a blurred and double vision effect that persists regardless of where one focuses their eyes.
Toxicity
Dihydrocodeine is characterized by a relatively low toxicity in relation to its dosage. Like all opiates, its long-term effects can vary and encompass diminished libido, apathy, and memory impairment. Some individuals may experience allergic reactions, such as skin swelling and rashes when using dihydrocodeine. Notably, it can become potentially lethal when combined with depressants like alcohol or benzodiazepines.
It is highly recommended to employ harm reduction practices when using this substance.
Tolerance and Addiction Potential
Similar to other opioids, chronic dihydrocodeine use carries a moderate level of addictiveness and a high potential for abuse, leading to psychological dependence in certain users. Once addiction takes hold, cravings and withdrawal symptoms may surface if usage is abruptly ceased.
Tolerance towards many of dihydrocodeine’s effects develops with prolonged and repeated use. The rate at which tolerance forms varies for different effects, with tolerance to constipation-inducing effects developing particularly slowly. Consequently, users may find themselves needing progressively larger doses to achieve the same effects. Subsequently, it takes approximately 3 to 7 days for tolerance to halve and 1 to 2 weeks to return to the baseline (in the absence of further consumption). Notably, dihydrocodeine induces cross-tolerance with all other opioids, implying that its consumption will decrease the effectiveness of other opioids.
Dangerous Interactions
Warning: Many psychoactive substances that are considered reasonably safe when used independently can become dangerous and potentially life-threatening when combined with certain other substances. The following list outlines some known dangerous interactions (though it may not cover all of them).
Always conduct independent research (e.g., consult sources like Google, DuckDuckGo, or PubMed) to ensure the safety of combining two or more substances. Some of the interactions listed below have been sourced from TripSit.
- Alcohol: Combining alcohol and dihydrocodeine amplifies the ataxia and sedation effects of both substances, potentially leading to sudden loss of consciousness at high doses. It’s crucial to place affected individuals in the recovery position to prevent aspiration in case of vomiting, and memory blackouts are likely.
- Amphetamines: Stimulants elevate respiration rates, allowing for higher opiate doses than would typically be used. However, if the stimulant wears off before the opiate, it may lead to respiratory arrest.
- Benzodiazepines: The combined use of benzodiazepines and dihydrocodeine can result in additive or synergistic central nervous system and respiratory-depressant effects, leading to rapid and unpredictable unconsciousness. Vomit aspiration is a risk if not placed in the recovery position, and memory loss or blackouts are common.
- Cocaine: Stimulants like cocaine can increase respiration rates, potentially allowing for higher opiate doses. However, if the stimulant wears off before the opiate, it may lead to respiratory arrest.
- DXM (Dextromethorphan): Generally considered toxic, combining DXM with dihydrocodeine can lead to central nervous system depression, breathing difficulties, heart problems, and liver toxicity. Additionally, DXM use can lower tolerance to opiates, intensifying their effects.
- GHB/GBL: These substances strongly and unpredictably potentiate each other, quickly leading to unconsciousness. When unconscious, there is a risk of vomit aspiration if the person is not placed in the recovery position.
- Ketamine: Both substances carry the risk of vomiting and unconsciousness. Suppose a user falls unconscious while under the influence; there is a severe risk of vomit aspiration if they are not placed in the recovery position.
- MAOIs (Monoamine Oxidase Inhibitors): Co-administration of MAOIs with specific opioids has been associated with rare reports of severe adverse reactions, including excitatory and depressive interactions. Symptoms may include agitation, headache, diaphoresis, hyperpyrexia, flushing, shivering, myoclonus, rigidity, tremor, diarrhoea, hypertension, tachycardia, seizures, and coma, and death has occurred in some cases.
- MXE (Methoxetamine): MXE can enhance opioid effects but also increase the risk of respiratory depression and organ toxicity when combined with dihydrocodeine.
- Nitrous: Combining nitrous oxide and dihydrocodeine potentiates the ataxia and sedation effects of both, potentially leading to sudden loss of consciousness at high doses. While unconscious, vomit aspiration is a risk if not placed in the recovery position, and memory blackouts are common.
- PCP (Phencyclidine): PCP may reduce opioid tolerance, increasing the risk of overdose.
- Tramadol: There is an increased risk of seizures when tramadol is combined with dihydrocodeine. Tramadol itself can induce seizures, and combining it with other opioids may lead to additive effects on seizure threshold. Additionally, central nervous system and respiratory-depressant effects may be additively or synergistically present.
- Grapefruit: While grapefruit itself is not psychoactive, it can affect the metabolism of certain opioids. Tramadol, oxycodone, and fentanyl, primarily metabolized by the enzyme CYP3A4, can be significantly inhibited by grapefruit juice. This may result in the drug taking longer to clear from the body and increase toxicity with repeated doses. Methadone may also be affected. CYP2D6 metabolizes codeine and hydrocodone, and individuals on medications that inhibit CYP2D6 or have a genetic mutation may not respond to codeine, as it cannot be metabolized into its active product, morphine.
Legal status
Austria: Dihydrocodeine is legally available for medical purposes under the AMG (Arzneimittelgesetz Österreich) but is considered illegal when sold or possessed without a prescription according to the SMG (Suchtmittelgesetz Österreich)
Australia: Dihydrocodeine is classified as a Schedule 3 medicine in Australia, which means it can be obtained without a prescription but is kept behind the pharmacy counter. Purchasers must consult with a pharmacist before obtaining it. The most common form available is an oral liquid called Rikodeine, with a dosage of 19mg/10mL, typically sold in 100 or 200mL bottles.
Germany: Dihydrocodeine is categorized as a controlled substance under Anlage III of the BtMG (Betäubungsmittelgesetz). It can only be prescribed using a narcotic prescription form. However, there is an exception for preparations that contain up to 2.5% or 100mg of dihydrocodeine per unit, which can be prescribed with a regular prescription unless the recipient is alcohol or drug-dependent.
Hong Kong: In Hong Kong, dihydrocodeine is regulated under Schedule 1 of the Dangerous Drugs Ordinance (Chapter 134). It can only be legally used by healthcare professionals and for university research purposes. Pharmacists can dispense dihydrocodeine when presented with a doctor’s prescription. The unauthorized supply of this substance can result in a fine of $10,000 (HKD), while trafficking or manufacturing carries a penalty of a $5,000,000 (HKD) fine and life imprisonment. Possession for personal consumption without a license from the Department of Health is illegal and may lead to a $1,000,000 (HKD) fine and a 7-year prison sentence.
Japan: In Japan, dihydrocodeine is available without a prescription and is used in cough medicines such as New Bron Solution-ACE. It is utilized as an antitussive in many products as an alternative to Dextromethorphan. Medications containing dihydrocodeine in Japan are often combined with caffeine to counteract sedative effects and discourage recreational use. The sale of cough medicines containing dihydrocodeine is restricted similarly to Dextromethorphan in the United States, with limits on purchase quantities and age restrictions, allowing purchases only for individuals aged 20 and older.[citation needed]
Russia: Dihydrocodeine is classified as a Schedule II controlled substance.
Sweden: Dihydrocodeine is available by prescription only.
Switzerland: Dihydrocodeine is classified as a controlled substance, specifically listed under Verzeichnis A. Medicinal use is permitted, with some preparations containing dihydrocodeine falling under Verzeichnis C, while others are excluded.
United Kingdom: In the United Kingdom, dihydrocodeine is categorized as a Class B drug. However, it can be obtained over the counter in limited quantities (less than 8 mg) when combined with paracetamol (as in co-dydramol). Dihydrocodeine is listed in Schedule 5 of the Misuse of Drugs Regulations 2001, exempting it from prohibition on possession if it is in the form of a single preparation not intended for injection and contains less than 100 mg (calculated as free base) or has a total concentration less than 2.5% (calculated as free base). Illegal possession of dihydrocodeine can result in up to 5 years in prison and a fine.
United States: In the USA, dihydrocodeine is classified as a DEA Schedule II substance. However, preparations containing small amounts of dihydrocodeine are categorized as Schedule III or Schedule V, depending on the concentration of dihydrocodeine relative to other active constituents, such as paracetamol (acetaminophen). This scheduling is similar to that in the UK. The DEA’s ACSCN for dihydrocodeine-free base and all salts is 9120, with an annual aggregate manufacturing quota of 250 kilos in 2013.
FAQ
1. What is Dihydrocodeine? Dihydrocodeine is a medication primarily used to relieve pain and suppress coughing. It belongs to the opioid analgesic class of drugs and is often prescribed in combination with other ingredients for various medical purposes.
2. How does Dihydrocodeine work? Dihydrocodeine works by binding to specific receptors in the brain and central nervous system, known as opioid receptors. This binding leads to reduced perception of pain and cough reflex suppression.
3. What medical conditions is Dihydrocodeine prescribed for? Dihydrocodeine is typically prescribed for the management of moderate to severe pain and as a cough suppressant. It may also be used for other conditions as determined by a healthcare provider.
4. Is Dihydrocodeine the same as codeine? No, Dihydrocodeine and codeine are different medications, although they both belong to the opioid class of drugs. Dihydrocodeine is a separate compound with distinct pharmacological properties and uses.
5. Is Dihydrocodeine safe to use? Dihydrocodeine can be safe and effective when used as prescribed by a healthcare professional. However, it can also be habit-forming and lead to addiction when misused. Always follow your healthcare provider’s instructions and do not exceed the recommended dose.
6. What are the potential side effects of Dihydrocodeine? Common side effects of Dihydrocodeine may include dizziness, drowsiness, constipation, nausea, and vomiting. Serious side effects such as difficulty breathing or an allergic reaction are rare but should be reported immediately to a healthcare provider.
7. Can I drink alcohol while taking Dihydrocodeine? It is generally not advisable to consume alcohol while taking Dihydrocodeine. Alcohol can enhance the sedative effects of the medication and increase the risk of side effects. Always consult with your healthcare provider regarding alcohol use while on this medication.
8. Is Dihydrocodeine safe during pregnancy and breastfeeding? Dihydrocodeine should only be used during pregnancy or breastfeeding under the guidance of a healthcare professional. It can pass into breast milk and potentially harm the baby.
9. Can I drive or operate heavy machinery while taking Dihydrocodeine? Dihydrocodeine can cause drowsiness and impair your ability to drive or operate machinery. It is essential to avoid such activities until you know how the medication affects you. Always follow your healthcare provider’s recommendations.
10. Is Dihydrocodeine available over-the-counter (OTC)? In many countries, Dihydrocodeine is available only by prescription due to its potential for misuse and dependence. Regulations regarding its availability may vary by region.
11. Can I stop taking Dihydrocodeine suddenly? Abruptly discontinuing Dihydrocodeine can lead to withdrawal symptoms. If you need to stop using the medication, it’s crucial to consult with your healthcare provider to develop a safe and gradual tapering plan.
12. What should I do if I suspect an overdose of Dihydrocodeine? An overdose of Dihydrocodeine can be life-threatening. If you or someone you know shows signs of an overdose, such as severe drowsiness, slow or shallow breathing, or loss of consciousness, seek immediate medical attention or call emergency services.
13. Can I take Dihydrocodeine with other medications? Dihydrocodeine may interact with other medications you are taking, potentially leading to adverse effects or reduced effectiveness. Always inform your healthcare provider about all the medications, supplements, and herbal products you are using to ensure safe and effective treatment.
14. How should I store Dihydrocodeine? Store Dihydrocodeine as directed on the medication label, typically at room temperature, away from moisture, heat, and direct sunlight. Keep it out of the reach of children and pets.
15. Where can I find more information about Dihydrocodeine? For comprehensive information about Dihydrocodeine, consult your healthcare provider pharmacist or refer to the medication’s package insert and prescribing information. It’s important to rely on reputable medical sources for accurate information.
References
- Multiple Sources of Information: The information presented here is compiled from various sources, including academic literature and official publications. It is essential to rely on credible sources for accurate and up-to-date information regarding the use of dihydrocodeine and its potential risks.
- Dihydrocodeine Metabolism: Dihydrocodeine is a medication commonly used for the treatment of moderate to severe pain. Its metabolism in the body involves the action of various enzymes, particularly cytochrome P450 enzymes. These enzymes play a crucial role in determining how the drug is processed and eliminated from the body.
- Active Metabolites: Dihydrocodeine is metabolized into active compounds that interact with opioid receptors in the brain. These interactions are responsible for the pain-relieving effects of the medication. Understanding the role of these metabolites is important in assessing the drug’s overall impact.
- Opioid Receptor Binding: Dihydrocodeine and its metabolites have affinities for specific opioid receptors in the central nervous system. These receptor interactions are central to the drug’s analgesic properties. It’s crucial to be aware of how dihydrocodeine affects these receptors when considering its use.
- Drug Interactions: Dihydrocodeine has the potential to interact with other substances, including alcohol and grapefruit juice. Combining dihydrocodeine with certain substances can lead to unexpected and potentially dangerous effects. Always consult with a healthcare provider or pharmacist to understand potential drug interactions.
- Regulatory Status: The legal status of dihydrocodeine varies by country. It is important to be aware of the regulations regarding its use and prescription requirements in your region. Misuse or unauthorized possession of dihydrocodeine can have legal consequences.
- Prescription Requirements: In many countries, dihydrocodeine is available only by prescription due to its potential for misuse and dependence. Regulations surrounding its availability, storage, and use may differ from one place to another.
- Medical Guidance: If you are prescribed dihydrocodeine, it’s essential to follow your healthcare provider’s instructions carefully. They can provide guidance on proper dosing, potential side effects, and how to manage pain effectively while minimizing risks.
- Driving and Machinery Operation: Dihydrocodeine can cause drowsiness and impairment of cognitive and motor skills. It is advisable to refrain from driving or operating heavy machinery until you know how the medication affects you.
- Pregnancy and Breastfeeding: If you are pregnant or breastfeeding, consult with your healthcare provider before taking dihydrocodeine, as it may have implications for the baby.
- Overdose and Withdrawal: Dihydrocodeine overdose can be life-threatening and should be treated as a medical emergency. Abruptly discontinuing the medication can lead to withdrawal symptoms, so consult with a healthcare provider for proper guidance if you need to stop taking it.
- Consult Reliable Sources: For comprehensive and specific information about dihydrocodeine, consult reputable sources such as healthcare professionals, pharmacists, or official patient information leaflets (PILs).
- Legal Consequences: Unauthorized possession or distribution of dihydrocodeine can have serious legal consequences. Be aware of the laws and regulations in your area regarding controlled substances.
- Stay Informed: Stay informed about the latest developments and guidelines related to dihydrocodeine by referring to official sources and medical literature.