Contents
Summary
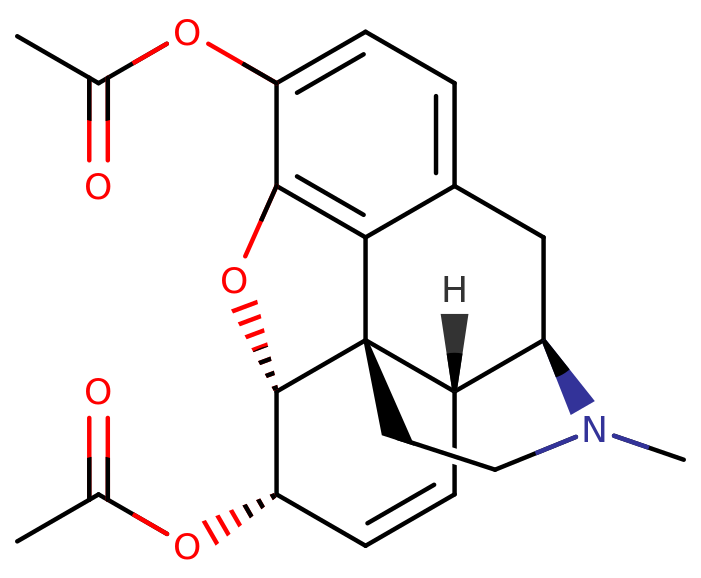
Heroin, recognized by various names, including diacetylmorphine and diamorphine, belongs to the morphinan opioid category and is derived from the dried latex of the Papaver somniferum plant. It is primarily sought after for its euphoric effects and is frequently used as a recreational drug. Medical-grade diamorphine, on the other hand, is administered as a pure hydrochloride salt. Illegally traded forms of heroin, found in white and brown powders worldwide, are often adulterated with cutting agents. Black tar heroin, another variation, is a blend of morphine derivatives, primarily 6-MAM (6-monoacetylmorphine), resulting from crude acetylation during the illicit production of street heroin.
Heroin serves a medical purpose in some countries for pain relief, such as during childbirth or in the treatment of conditions like heart attacks, as well as in opioid replacement therapy.
Typically, it is administered through injection, commonly intravenously, although it can also be snorted, smoked, or inhaled. In a clinical context, intravenous injection is the most frequent route of administration, although it may also be delivered intramuscularly, subcutaneously, or orally in tablet form. The onset of its effects is typically rapid, lasting for a few hours.
Common side effects encompass reduced respiration (breathing), dry mouth, drowsiness, impaired cognitive function, constipation, and the risk of addiction. Injection use can lead to complications such as abscesses, infected heart valves, blood-borne infections, and pneumonia. Following extended use, opioid withdrawal symptoms can manifest within hours of the last dose. When injected intravenously, heroin is two to three times more potent than a comparable dose of morphine. It typically presents in the form of white or brown powder.
Heroin addiction treatment commonly involves a combination of behavioural therapy and medications. Medications used may include buprenorphine, methadone, or naltrexone. In cases of heroin overdose, naloxone can be administered as an antidote. As of 2015, an estimated 17 million people were using opiates, with heroin being the most prevalent among them, and opioid use was linked to 122,000 deaths. The global heroin user population, as of 2015, was believed to have risen in Africa, the Americas, and Asia since 2000. In the United States, approximately 1.6 per cent of the population has used heroin at some point. Notably, opioid overdoses, often involving heroin, are a leading cause of drug-related fatalities.
Heroin was first synthesized by C. R. Alder Wright in 1874 using morphine, a natural compound derived from the opium poppy.[20] Internationally, heroin is categorized under Schedules I and IV of the Single Convention on Narcotic Drugs, making its production, possession, and sale illegal without the requisite licenses. In 2016, approximately 448 tons of heroin were manufactured. Afghanistan, in 2015, contributed to around 66% of the world’s opium production. Illicit heroin is frequently adulterated with other substances like sugar, starch, caffeine, quinine, or other opioids such as fentanyl.
| Identifiers | |
|---|---|
| IUPAC name | |
| CAS Number | 561-27-3 HCl: 1502-95-0 |
|---|---|
| PubChem CID | 5462328 |
| DrugBank | DB01452 |
| ChemSpider | 4575379 |
| UNII | 70D95007SXHCl: 8H672SHT8E |
| KEGG | D07286 |
| ChEBI | CHEBI:27808 |
| ChEMBL | ChEMBL459324 |
| CompTox Dashboard (EPA) | DTXSID6046761 |
| ECHA InfoCard | 100.008.380 |
| Chemical and physical data | |
| Formula | C21H23NO5 |
| Molar mass | 369.417 g·mol−1 |
Uses
Bayer’s initial trade name for heroin is predominantly employed in non-medical contexts, serving as a recreational substance cherished for its capacity to induce euphoria. Anthropologist Michael Agar once coined heroin as “the perfect whatever drug.” Rapidly, tolerance to its effects ensues, necessitating escalated doses for the desired outcomes. Its appeal among recreational drug users, in contrast to morphine, often stems from its perceived distinct effects.
Short-term addiction studies conducted by the same researchers have demonstrated that tolerance develops at a similar rate for both heroin and morphine. When compared to other opioids like hydromorphone, fentanyl, oxycodone, and pethidine (meperidine), former addicts displayed a pronounced preference for heroin and morphine, implying that these substances are particularly prone to misuse and the development of dependence. Moreover, morphine and heroin exhibited a much greater propensity to induce euphoria and other “positive” subjective effects when juxtaposed with these other opioids.
Medical Uses
In the United States, heroin is not sanctioned for medical purposes.
Under the generic name diamorphine, heroin is prescribed as a potent pain-relieving medication in the United Kingdom, with various administration routes, including oral, subcutaneous, intramuscular, intrathecal, intranasal, or intravenous. It is indicated for the treatment of acute pain, such as that resulting from severe physical trauma, myocardial infarction, post-surgical pain, and chronic pain associated with end-stage terminal illnesses. In other countries, morphine or alternative potent opioids are more commonly employed in similar scenarios. In 2004, the National Institute for Health and Clinical Excellence issued guidance for caesarean section management, recommending the use of intrathecal or epidural diamorphine for post-operative pain relief. Women who have received intrathecal opioids should undergo close hourly monitoring of respiratory rate, sedation, and pain scores for at least 12 hours with diamorphine and 24 hours with morphine. Diamorphine is recommended (0.3–0.4 mg intrathecally) for intra- and postoperative analgesia as it reduces the requirement for supplementary analgesia following a caesarean section. Epidural diamorphine (2.5–5 mg) is a suitable alternative.
Diamorphine remains widely used in palliative care in the UK, often administered subcutaneously, especially via a syringe driver for patients unable to swallow morphine solution easily. Diamorphine boasts a greater fat solubility and, consequently, higher potency when injected, thus requiring smaller doses for equivalent pain relief. These attributes are advantageous for delivering high doses of opioids via the subcutaneous route, often a necessity in palliative care.
The substance is also employed in the palliative management of bone fractures and other traumas, particularly in children. In the context of trauma, it is primarily administered nasally in hospital settings, with prepared nasal sprays available. Traditionally, it was prepared by attending physicians, often from the same “dry” ampoules used for injection. In children, Ayendi nasal spray is available in doses of 720 micrograms and 1600 micrograms per 50 microlitres actuation of the spray. This offers a non-invasive alternative in pediatric care, eliminating the fear of injections in children.
Maintenance Therapy
A number of European countries prescribe heroin for the treatment of heroin addiction. The initial Swiss HAT (Heroin-assisted treatment) trial (“PROVE” study) involved approximately 1,000 participants in 18 treatment centres between 1994 and 1996. By the end of 2004, 1,200 patients were enrolled in HAT across 23 treatment centres in Switzerland. Diamorphine may be used as a maintenance medication to support the treatment of opiate addiction, typically in long-term chronic intravenous (IV) heroin users. It is only prescribed after exhaustive attempts at treatment through other means. Contrary to the perception that heroin users can effortlessly obtain a prescription, the process takes several weeks before a prescription for diamorphine is issued. While this approach remains somewhat controversial among proponents of a zero-tolerance drug policy, it has proven more effective than methadone in enhancing the social and health conditions of addicts.
The UK Department of Health’s Rolleston Committee Report in 1926 established the British practice of prescribing diamorphine to users, which persisted for four decades. Dealers were prosecuted, but doctors could prescribe diamorphine to users in the withdrawal process. In 1964, the Brain Committee recommended that only selected approved doctors operating in approved specialized centres be permitted to prescribe diamorphine and cocaine to users. The law became more stringent in 1968. Starting in the 1970s, the emphasis shifted towards abstinence and the use of methadone. Currently, only a small number of users in the UK are prescribed diamorphine.
In 1994, Switzerland initiated a trial diamorphine maintenance program for users who had previously failed multiple withdrawal programs. The aim was to safeguard users’ health by mitigating medical issues arising from illicit diamorphine use. The first trial in 1994 involved 340 users, and enrollment was later expanded to 1000, given the apparent success of the program. The trials demonstrated that diamorphine maintenance was superior to other treatment methods in improving the social and health circumstances of this patient group. Additionally, it proved to be cost-effective, as it significantly reduced expenses associated with trials, incarceration, healthcare interventions, and delinquency. Patients are required to visit a treatment centre twice daily, where they inject their prescribed dose of diamorphine under medical supervision. They are also responsible for contributing approximately 450 Swiss francs per month toward treatment costs. A national referendum in November 2008 garnered 68% support for introducing diamorphine prescription into federal law, replacing the previous time-limited executive ordinances. The success of the Swiss trials prompted German, Dutch, and Canadian cities to implement their diamorphine prescription programs. Some Australian cities, including Sydney, have established legal diamorphine supervised injecting centres, aligning with broader harm minimization initiatives.
Since January 2009, Denmark has prescribed diamorphine to a few addicts who had previously failed with methadone and buprenorphine treatments. Starting in February 2010, addicts in Copenhagen and Odense became eligible to receive free diamorphine. Later that year, other cities, including Århus and Esbjerg, joined the program. Approximately 230 addicts were expected to benefit from free diamorphine. Danish addicts, however, can only inject heroin according to the guidelines set by the Danish National Board of Health. Approximately 900 of the estimated 1500 drug users who did not respond to the existing oral substitution treatment would not be eligible for treatment with injectable diamorphine, either due to extensive use of non-opioids or their reluctance to undergo injectable diamorphine treatment.
In July 2009, the German Bundestag passed a law allowing diamorphine prescription as a standard treatment for addicts, following the authorization of a large-scale diamorphine prescription trial in the country in 2002.
On 26 August 2016, Health Canada issued regulations amending prior regulations it had issued under the Controlled Drugs and Substances Act. These amendments, known as the “New Classes of Practitioners Regulations,” the “Narcotic Control Regulations,” and the “Food and Drug Regulations,” authorized doctors to prescribe diamorphine to individuals with severe opioid addiction who had not responded to other treatments. This prescription heroin can be obtained by doctors through Health Canada’s Special Access Programme (SAP), designed for “emergency access to drugs for patients with serious or life-threatening conditions when conventional treatments have failed, are unsuitable, or are unavailable.”

Routes of administration
The onset of heroin’s effects varies depending on how it’s taken. Smoking delivers the fastest results, though intravenous injection leads to a more rapid increase in blood concentration. This is followed by suppository (anal or vaginal insertion), insufflation (snorting), and ingestion (swallowing).
A study from 2002 suggests that a fast onset of action enhances the addictive nature of drugs. Ingesting heroin doesn’t produce the intense rush that’s a precursor to the high experience with intravenous use. The rush from injection can occur in seconds, while oral administration takes about half an hour to produce the high. Therefore, the higher the dosage and the faster the route of administration, the greater the potential risk for psychological dependence and addiction.
Large doses of heroin can lead to fatal respiratory depression, and the drug has been used for suicide or as a murder weapon. Serial killer Harold Shipman used diamorphine on his victims, prompting tighter regulations on the storage, prescription, and disposal of controlled drugs in the UK following the Shipman Inquiry.
Because tolerance to respiratory depression develops quickly with continued use and dissipates just as swiftly during withdrawal, it’s often challenging to determine whether a heroin overdose was accidental, suicidal, or homicidal. This situation is exemplified by overdose deaths like those of Sid Vicious, Janis Joplin, Tim Buckley, Hillel Slovak, Layne Staley, Bradley Nowell, Ted Binion, and River Phoenix.
By Mouth:
Oral heroin use is less common because it lacks the intense rush and potency of other methods. Heroin is converted to morphine through first-pass metabolism when ingested. Heroin’s oral bioavailability varies with dosage, reaching up to 64.2% for high doses and 45.6% for low doses. Opiate-naive users have lower absorption rates, up to 22.9%. Morphine’s maximum plasma concentration following oral heroin is about twice that of oral morphine.
Injection:
Injection, also known as “slamming,” carries greater risks than other methods. Heroin base in Europe requires an acid (usually citric acid or lemon juice) and heat to dissolve, while the east-coast US has heroin in hydrochloride salt form, needing only water. Users initially inject in arm veins but may turn to more dangerous areas as these veins collapse, potentially leading to deep vein thrombosis. Sharing needles or equipment can transmit blood-borne diseases like HIV/AIDS or hepatitis.
Smoking:
Smoking heroin involves vaporizing it and inhaling the fumes, often using glass pipes or aluminium foil. It can also be inhaled through rolled-up foil, known as “chasing the dragon.”
Insufflation:
Users can snort finely crushed heroin to experience a quicker onset and higher bioavailability than oral administration. However, this route doesn’t produce the intense rush associated with injection.
Suppository:
Little research has focused on the suppository (anal or vaginal insertion) methods, also called “plugging.” This is typically done using an oral syringe. The drug is dissolved in the syringe, lubricated, and inserted into the anus or vagina, where the drug is absorbed through the lining membranes.
Adverse effects
Heroin is categorized as a highly potent and harmful drug. Similar to most opioids, pure heroin can result in adverse effects. The purity of street heroin can vary significantly, leading to overdoses when its purity is unexpectedly high.
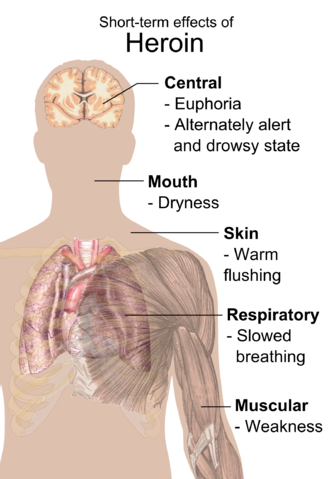
Short-term Effects:
Individuals who use heroin in the short term commonly report experiencing an intense rush characterized by an acute, transcendent state of euphoria. This occurs while diamorphine is metabolized into 6-monoacetylmorphine (6-MAM) and morphine in the brain. Some argue that heroin produces more euphoria compared to other opioids, possibly due to the presence of 6-MAM, a unique heroin metabolite. However, clinical studies comparing the physiological and subjective effects of injected heroin and morphine in individuals previously addicted to opioids found no preference for one drug over the other. Equipotent doses of both drugs produced similar effects, with no significant difference in self-reported feelings of euphoria, ambition, nervousness, relaxation, drowsiness, or sleepiness.
The rush is typically accompanied by a warm flushing of the skin, a dry mouth, and a sensation of heaviness in the limbs. Nausea, vomiting, and severe itching can also occur. After the initial effects, users often experience drowsiness for several hours, clouded mental function, slowed heart function, and significantly reduced breathing, which can become life-threatening. Slow breathing can even lead to coma and permanent brain damage. Heroin use has also been linked to myocardial infarction (heart attacks).
Long-term Effects:
Long-term intravenous heroin use, mainly due to contaminants found in illegal heroin and unsterile needles, can have severe consequences. Repeated heroin use can alter the brain’s physical structure and physiology, resulting in long-term imbalances in neuronal and hormonal systems that are challenging to reverse. Studies have indicated deterioration in the brain’s white matter due to heroin use, potentially affecting decision-making abilities, behaviour regulation, and responses to stress.
Heroin use also leads to significant tolerance and physical dependence. Tolerance means that increasing amounts of the drug are needed to achieve the same effects, while physical dependence results in withdrawal symptoms if drug use is abruptly reduced.
Injection:
Intravenous heroin use with needles and syringes or shared equipment can lead to several health risks, including:
- Contracting blood-borne diseases like HIV and hepatitis due to needle sharing.
- Developing bacterial or fungal endocarditis and possibly venous sclerosis.
- Developing abscesses.
- Experiencing poisoning from contaminants added to “cut” or diluted heroin.
- Experiencing decreased kidney function (nephropathy), although it’s unclear whether this is due to impurities or infectious diseases.
Withdrawal:
Heroin withdrawal syndrome can begin as soon as two hours after discontinuing the drug, but the timing can vary depending on tolerance and the last consumed dose. Withdrawal symptoms may include sweating, malaise, anxiety, depression, restlessness, the sensitivity of the genitals in females, a sense of heaviness, excessive yawning or sneezing, runny nose, insomnia, cold sweats, chills, severe muscle and bone aches, nausea, vomiting, diarrhoea, cramps, watery eyes, fever, cramp-like pains, and involuntary limb spasms (the origin of the term “kicking the habit”).
Overdose
Heroin overdose is typically managed with the opioid antagonist naloxone, which effectively reverses the heroin’s effects and quickly restores consciousness. However, naloxone administration may lead to withdrawal symptoms. Naloxone has a shorter half-life than some opioids, so it might need to be administered multiple times until the body fully metabolizes the opioid.
Between 2012 and 2015, heroin was the leading cause of drug-related deaths in the United States. Since then, fentanyl has become a more common cause of drug-related fatalities.
The time it takes for a fatal overdose to occur can vary from several minutes to several hours, depending on drug interactions and various factors. Death typically results from a lack of oxygen due to suppressed breathing caused by the opioid. Heroin overdoses can happen due to unexpected increases in dose or purity or reduced opioid tolerance. However, many reported overdose deaths are likely the result of interactions with other depressant drugs like alcohol or benzodiazepines. Since heroin can induce nausea and vomiting, some overdose deaths attributed to heroin are caused by the inhalation of vomit by an unconscious individual.
The median lethal dose for an average 75 kg opiate-naive person is estimated to be between 75 and 600 mg, though illicit heroin’s purity is highly variable and unpredictable. This means users may unintentionally take much more than intended when preparing what they consider a moderate dose. Additionally, tolerance typically decreases after a period of abstinence. If a user takes a dose similar to their previous use after tolerance has decreased, they may experience much stronger drug effects, potentially leading to an overdose. There is speculation that some heroin-related deaths could be the result of overdose or allergic reactions to quinine, which is sometimes used as a cutting agent in heroin.
Pharmacology
When consumed orally, heroin undergoes extensive first-pass metabolism through deacetylation, essentially functioning as a prodrug for delivering morphine into the systemic circulation. However, when the drug is administered via injection, it bypasses this initial metabolic process. This rapid entry into the bloodstream is facilitated by the acetyl groups, which make heroin significantly more fat-soluble than morphine itself, allowing it to cross the blood-brain barrier swiftly. Once within the brain, heroin is enzymatically deacetylated, first into the inactive form 3-monoacetylmorphine and the active form 6-monoacetylmorphine (6-MAM). Subsequently, these compounds are further metabolized into morphine. These morphine molecules then bind to μ-opioid receptors, giving rise to the drug’s euphoric, analgesic (pain-relief), and anxiolytic (anti-anxiety) effects. It’s worth noting that heroin itself exhibits a relatively low affinity for the μ receptor. The analgesic effect occurs as a result of the activation of the μ receptor G-protein coupled receptor, which indirectly hyperpolarizes neurons, reducing the release of pain-related neurotransmitters, thereby providing pain relief and an increased tolerance to pain.
However, unlike hydromorphone and oxymorphone, when administered intravenously, heroin induces a more pronounced release of histamine, similar to morphine. This leads to a heightened subjective “body high” for some users but can also result in itching (pruritus) during initial use.
Typically, GABA, a neurotransmitter released by inhibitory neurons, suppresses the release of dopamine. Opiates such as heroin and morphine diminish the inhibitory activity of these neurons, causing an increase in dopamine release in the brain. This surge in dopamine is responsible for the euphoric and rewarding effects of heroin.
Both morphine and 6-MAM act as μ-opioid agonists, binding to receptors found throughout the brain, spinal cord, and gastrointestinal tract in all mammals. The μ-opioid receptor also binds to endogenous opioid peptides like β-endorphin, Leu-enkephalin, and Met-enkephalin. Repeated heroin use leads to physiological changes, including an increase in the production of μ-opioid receptors (upregulation). These physiological adaptations result in tolerance and dependence, meaning that discontinuing heroin use results in uncomfortable symptoms such as pain, anxiety, muscle spasms, and insomnia, collectively known as opioid withdrawal syndrome. The onset of withdrawal symptoms can occur between 4 to 24 hours after the last heroin dose, depending on usage. Morphine also binds to δ- and κ-opioid receptors.
There is evidence suggesting that 6-MAM binds to a subtype of μ-opioid receptors that are also activated by the morphine metabolite morphine-6β-glucuronide but not by morphine itself. A third subtype of μ-opioid receptors, known as the mu-3 receptor, might also be influenced by other six-position monoesters of morphine. However, the exact contribution of these receptors to the overall pharmacology of heroin remains uncertain.
A subgroup of morphine derivatives, specifically the 3,6 esters of morphine, which have similar effects and uses, includes the clinically employed potent analgesics nicomorphine (Vilan) and dipropanoylmorphine. There is also a dihydromorphine analogue of the latter, diacetyldihydromorphine (Paralaudin). Two other 3,6 diesters of morphine, dibenzoylmorphine and acetylpropionylmorphine, were created alongside diamorphine in 1874–75. They were marketed as substitutes after diamorphine was prohibited in 1925 and were sold as the earliest “designer drugs” until being banned by the League of Nations in 1930.
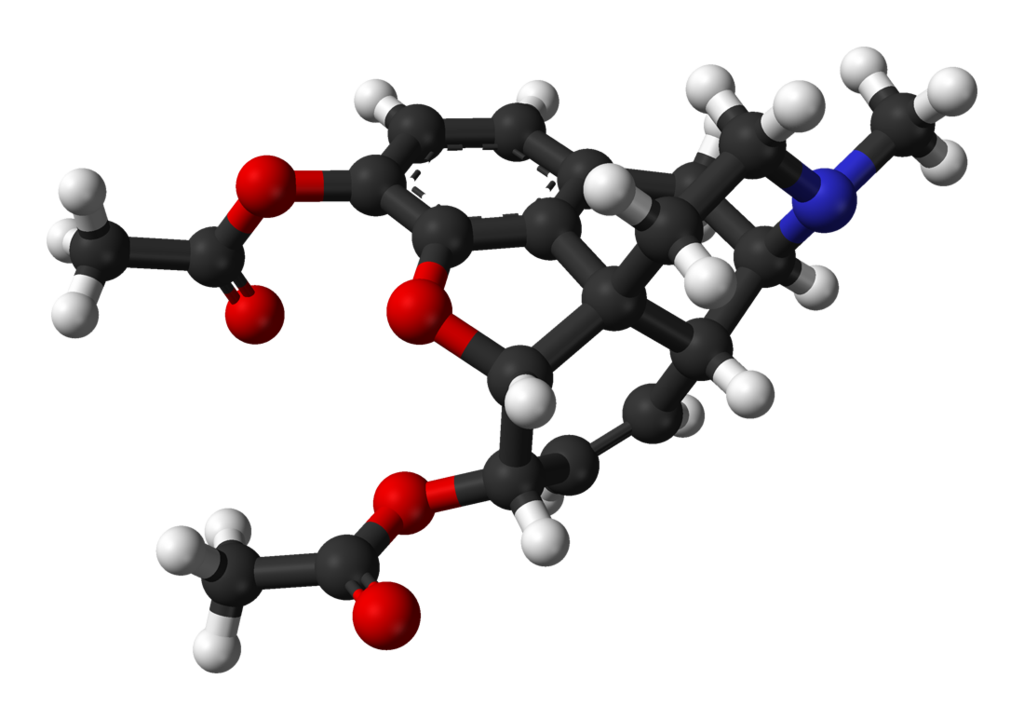
Chemistry
Diamorphine is synthesized by acetylating morphine obtained from natural opium sources, typically using acetic anhydride.
The primary metabolites of diamorphine, namely 6-MAM, morphine, morphine-3-glucuronide, and morphine-6-glucuronide, can be measured in blood, plasma, or urine for various purposes such as monitoring usage, confirming poisoning diagnoses, or aiding in forensic investigations related to deaths. Most commercial opiate screening tests notably cross-react with these metabolites, along with other biotransformation products that may be present after consuming street-grade diamorphine, such as 6-monoacetylcodeine and codeine. However, chromatographic techniques can readily differentiate and quantify each of these substances. When interpreting test results, it’s crucial to consider the individual’s history of diamorphine use since chronic users can develop tolerance to doses that would incapacitate someone who is opiate-naive. Additionally, chronic users often have elevated baseline levels of these metabolites in their system. Furthermore, certain testing methods involve a hydrolysis step before quantification, which converts many of the metabolic products into morphine, potentially yielding a result that is twice as large as a method that assesses each product individually.
History
The cultivation of the opium poppy dates back to as early as 3400 BC in lower Mesopotamia. In the 19th century, chemical analysis of opium revealed that its effects could be attributed mainly to the alkaloids codeine and morphine.
Diamorphine was initially synthesized in 1874 by C. R. Alder Wright, a British chemist at St. Mary’s Hospital Medical School in London. He had been conducting experiments involving the combination of morphine with various acids. Through a process that involved boiling anhydrous morphine alkaloid with acetic anhydride for an extended period, he created a more potent, acetylated form of morphine, which is now known as diacetylmorphine or morphine diacetate. Wright sent this compound to F. M. Pierce at Owens College in Manchester for analysis. Pierce reported back to Wright:
“Doses… were subcutaneously injected into young dogs and rabbits, resulting in the following general observations: marked prostration, fear, and rapid onset of sleepiness following the administration. The animals displayed sensitivity in their eyes, constricted pupils, substantial salivation in dogs, and occasional bouts of vomiting. While respiration initially became accelerated, it later slowed down, and the heart’s activity diminished, becoming irregular. There was a notable loss of coordination in muscular movements, weakness in the pelvic and hind limbs, and a decrease in rectal temperature by about 4°.”
Wright’s discovery did not lead to further developments, and it wasn’t until 23 years later that chemist Felix Hoffmann independently resynthesized diamorphine. Hoffmann was working at the pharmaceutical company Bayer in Elberfeld, Germany, under the guidance of his supervisor Heinrich Dreser. Dresser instructed Hoffmann to acetylate morphine with the intention of producing codeine, an opium poppy constituent that had similar pharmacological effects to morphine but was less potent and less addictive. Surprisingly, the experiment resulted in an acetylated form of morphine that was one and a half to two times more potent than morphine itself. Hoffmann successfully synthesized heroin on August 21, 1897, just eleven days after he had synthesized aspirin.
The head of Bayer’s research department is credited with coining the drug’s name, “heroin,” derived from the German word “heroisch,” meaning “heroic” or “strong” (originating from the ancient Greek word “heroes, ήρως”). Bayer’s scientists were not the first to create heroin, but they found ways to manufacture it, and Bayer played a leading role in its commercialization.
Bayer marketed diacetylmorphine under the trademark name “Heroin” as an over-the-counter drug. It was primarily developed as a morphine substitute for cough suppressants, aiming to offer a non-addictive alternative to morphine, which was a popular recreational drug at the time. However, contrary to Bayer’s claim of being a “non-addictive morphine substitute,” heroin would eventually become one of the most addictive substances among its users.
From 1898 to 1910, diamorphine was marketed as “Heroin,” both as a non-addictive morphine substitute and as a cough suppressant.[93] The 11th edition of the Encyclopædia Britannica (1910) noted: “In the cough of phthisis, minute doses of morphine are beneficial, but in this particular disease, morphine is frequently replaced by codeine or heroin, which effectively suppress irritating coughs without causing the narcotic effects associated with morphine.”
In the United States, the Harrison Narcotics Tax Act was enacted in 1914 to regulate the sale and distribution of diacetylmorphine and other opioids. This allowed the drug to be prescribed and sold for medical purposes. However, in 1924, the United States Congress banned its sale, importation, and manufacturing. It is currently classified as a Schedule I substance, making it illegal for non-medical use in countries that are signatories to the Single Convention on Narcotic Drugs treaty, including the United States.
In 1925, the Health Committee of the League of Nations prohibited diacetylmorphine, although it took over three years for this ban to be enforced. During this time, the first designer drugs, including 3,6 diesters and 6 monoesters of morphine, as well as acetylated analogues of closely related drugs like hydromorphone and dihydromorphine, were produced in large quantities to meet the global demand for diacetylmorphine. This continued until 1930 when the Committee banned diacetylmorphine analogues that offered no therapeutic advantage over already-used drugs. This marked one of the first major legislative actions in this regard.[citation needed]
Bayer lost some of its trademark rights to heroin (as well as aspirin) under the 1919 Treaty of Versailles following Germany’s defeat in World War I.
Heroin use, particularly among jazz musicians, became prevalent in the mid-20th century. Notable users included Billie Holiday, saxophonists Charlie Parker and Art Pepper, guitarist Joe Pass, and pianist/singer Ray Charles. A significant number of jazz musicians struggled with addiction. Heroin use also became a problem for many rock musicians, particularly from the late 1960s through the 1990s. Musicians like Pete Doherty, Kurt Cobain of Nirvana, Phil Anselmo of Pantera, James Taylor, Jimmy Page, John Lennon, Eric Clapton, Johnny Winter, Keith Richards, and Janis Joplin were known to have used heroin. Several songs have been composed referencing heroin use.
Society and culture
Names
The Recommended International Nonproprietary Name and British Approved Name for diamorphine is “Diamorphine.” Heroin goes by various synonyms, including diacetylmorphine and morphine diacetate. On the streets, it’s known by a multitude of names such as dope, H, smack, junk, horse, scag, and brown, among others.
Legal Status
Asia:
In Hong Kong, diamorphine falls under Schedule 1 of the Dangerous Drugs Ordinance, Chapter 134, and is available only by prescription. An unlawful supply of diamorphine can lead to a hefty fine of $5,000,000 (HKD) and life imprisonment. The penalty for trafficking or manufacturing diamorphine includes a $5,000,000 (HKD) fine and life imprisonment. Possessing diamorphine without a Department of Health license is illegal and carries a $1,000,000 (HKD) fine and a 7-year jail term.
Europe:
In the Netherlands, diamorphine is classified as a List I drug under the Opium Law. It can be prescribed only under strict regulation for long-term addicts for whom methadone treatment has failed. It is not used for treating severe pain or other illnesses.
In the United Kingdom, diamorphine is available by prescription but is classified as a restricted Class A drug. It may be used for treating acute pain, myocardial infarction, acute pulmonary oedema, and chronic pain, but a specialist must supervise the latter. The British National Formulary (BNF) 50th edition notes that all opioid analgesics lead to dependence and tolerance, but this does not deter their use in controlling pain in terminal illness. In palliative care for cancer patients, diamorphine is often administered using a syringe driver.
In Switzerland, heroin is produced in injectable or tablet form, known as Diaphin, by a private company under a government contract. Swiss-produced heroin has been imported into Canada with government approval.
Australia:
In Australia, diamorphine is listed as a Schedule 9 prohibited substance under the Poisons Standard as of October 2015. A Schedule 9 drug is defined as “Substances which may be abused or misused, the manufacture, possession, sale, or use of which should be prohibited by law except when required for medical or scientific research, or analytical, teaching, or training purposes with approval of the CEO.”
North America:
In Canada, diamorphine is a controlled substance under Schedule I of the Controlled Drugs and Substances Act (CDSA). Obtaining diamorphine without disclosing authorization 30 days prior to getting another prescription is an indictable offence subject to imprisonment for up to seven years. Possession of diamorphine for trafficking is also an indictable offence carrying a possible life imprisonment sentence.
In the United States, diamorphine is classified as a Schedule I drug as per the Controlled Substances Act of 1970, making it illegal to possess without a DEA license. Possession of more than 100 grams of diamorphine or a mixture containing diamorphine is punishable with a minimum mandatory sentence of 5 years in federal prison.
In 2021, the state of Oregon became the first in the U.S. to decriminalize heroin use following the passage of Ballot Measure 110 in 2020. This measure allows individuals with small amounts of heroin to avoid arrest.
Turkey:
Turkey maintains strict laws against the use, possession, or trafficking of illegal drugs. Offenders can face heavy fines or prison sentences ranging from 4 to 24 years.
Misuse of Prescription Medication:
Misuse of prescription medications, including opioids, can lead to heroin use and dependence. The rise in deaths from illegal opioid overdoses often follows an increase in deaths caused by prescription opioid overdoses. Prescription opioids are relatively easy to obtain, potentially pushing users toward heroin use, as it is often cheaper than prescription pills.
Economics
Production:
Diamorphine is derived from the acetylation of morphine obtained from natural opium sources. The production process involves isolating the water-soluble components of raw opium, including morphine, in a strongly basic aqueous solution. Subsequently, the morphine base is recrystallized through the addition of ammonium chloride. The solid morphine base is then separated. To form heroin, the morphine base is reacted with acetic anhydride. The resulting brown heroin base is typically impure and may undergo further purification steps, resulting in a white or differently coloured product. Heroin purity is categorized into four grades, with No.4 being the purest form and No.1 and No.2 representing unprocessed raw heroin.
Trafficking:
International Drug Routes:
Heroin trafficking is a global issue, with Afghanistan being the largest producer, accounting for 87% of the world’s diamorphine production, according to a U.N.-sponsored survey in 2004. Opium production in Afghanistan has been linked to around 100,000 deaths annually. Various factors, including the cultivation of opium in different regions, such as Southeast Asia and the Golden Triangle, have influenced the trade. Heroin trafficking routes have shifted over time, involving different criminal organizations and countries, with the Sinaloa Cartel being a significant player in smuggling heroin into the United States. Other destinations for Afghan opiates include Russia, Europe, and Iran.
Trafficking in heroin carries severe penalties in some countries, including the death penalty in parts of Southeast Asia and the Middle East. These penalties may apply even to citizens of countries where such penalties are not in place, causing diplomatic controversies. The trade has a long history, originating from strict regulations on opium and heroin production in the early 1900s, which led to illegal trade between countries. Over time, heroin labs emerged in various regions, including China, and Chinese triad gangs played a significant role in the illicit trade. The French Connection route, which started in the 1930s, contributed to the international spread of heroin production. The dynamics of the trade changed during and after World War II, with a resurgence of production in regions like Sicily and Italy. The postwar Italian government’s weakness allowed the Mafia to set up heroin labs in Sicily, located along the historic trade route for opium. The trade also saw increased production during the Soviet-Afghan war and the development of the Golden Triangle opium production region.
Street Price:
The retail price of brown heroin varies across Europe, ranging from €14.5 per gram in Turkey to €110 per gram in Sweden, with most countries reporting typical prices of €35–40 per gram. White heroin prices, available in a few European countries, range between €27 and €110 per gram. In the United States, typical retail prices are reported at US$172 per gram.
Harm Reduction:
Harm reduction strategies aim to minimize the negative consequences associated with drug use, including heroin. These strategies focus on promoting safer ways of consuming the drug, such as smoking, nasal use, or oral/rectal insertion, to reduce the risks of overdose and infections linked to injecting. Users are advised to start with small amounts of the drug to assess its strength and minimize overdose risks. Harm reduction initiatives also include distributing new needles, syringes, and other equipment to reduce the transmission of blood-borne infections among injecting drug users. Safe injection sites, found in some countries, allow users to inject heroin under medical supervision. These sites aim to engage with difficult-to-reach users and provide access to health services.
FAQ
1. What is heroin?
Heroin, also known as diamorphine, is a powerful and illegal opioid drug derived from morphine, which, in turn, is derived from the opium poppy plant. It is classified as a Schedule I controlled substance in many countries due to its highly addictive nature and potential for abuse.
2. How is heroin used?
Heroin is typically used by injecting it into the veins, but it can also be smoked or snorted. Injecting heroin is known as “shooting up,” while smoking it is called “chasing the dragon.” Regardless of the method of use, heroin rapidly enters the brain and produces intense feelings of euphoria and relaxation.
3. What are the short-term effects of heroin use?
Short-term effects of heroin use include a rush of euphoria, warm flushing of the skin, dry mouth, heavy limbs, and clouded mental functioning. Users often experience a “nodding” state where they alternate between being awake and tired. Heroin use also depresses the central nervous system, leading to slowed breathing and heart rate.
4. What are the long-term effects of heroin use?
Long-term heroin use can result in numerous health issues, including addiction, collapsed veins (from injecting), damaged nasal tissue (from snorting), bacterial infections, and abscesses. Chronic use can also lead to liver and kidney disease, respiratory problems, and mental health disorders.
5. Can heroin be used safely?
No, there is no safe or controlled way to use heroin. It is an illicit and highly addictive drug with severe health risks. Even a single use can lead to addiction, overdose, or other life-threatening complications.
6. How addictive is heroin?
Heroin is one of the most addictive substances known. Many people become physically and psychologically dependent on it after just a few uses. The withdrawal symptoms can be excruciating, which often drives users to continue taking the drug to avoid the pain of withdrawal.
7. What are the signs of heroin addiction?
Signs of heroin addiction may include neglecting responsibilities, social withdrawal, financial problems, a decline in personal hygiene, track marks (if injected), and a preoccupation with obtaining and using the drug. Individuals addicted to heroin may also experience severe mood swings.
8. Is there treatment available for heroin addiction?
Yes, there are treatment options available for heroin addiction. These include medication-assisted treatment (MAT), counselling, therapy, and support groups. MAT uses medications like methadone or buprenorphine to reduce cravings and withdrawal symptoms, making it easier for individuals to quit using heroin.
9. What are the risks of a heroin overdose?
Heroin overdoses can be fatal. Signs of overdose include slow, shallow breathing, pinpoint pupils, blue lips or fingertips, and unconsciousness. If someone is suspected of overdosing on heroin, immediate medical attention is crucial. Naloxone (Narcan) is a medication that can reverse the effects of an opioid overdose and is often used in emergencies.
10. Is there any safe way to use heroin?
No, there is no safe way to use heroin. Using this drug is associated with significant health risks, addiction, and potentially fatal consequences. The best way to avoid these risks is not to use heroin or to seek help if you or someone you know is struggling with addiction.
11. Why is heroin use so dangerous?
Heroin is dangerous due to its high potential for addiction, overdose, and a wide range of health risks associated with its use. It alters brain chemistry and can lead to severe physical and mental health problems, making it one of the most hazardous illicit drugs in the world.
12. Where can I find help for heroin addiction?
If you or someone you know is struggling with heroin addiction, it’s essential to seek help immediately. You can start by contacting local addiction treatment centres, seeking assistance from a healthcare provider, or contacting a helpline like the Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 1-800-662-HELP (4357) in the United States. Reaching out for support is a critical step toward recovery.
References
- Sweetman SC, editor. Martindale: The Comprehensive Drug Reference (36th ed.). London: Pharmaceutical Press; 2009. Page 42. ISBN 978-0-85369-840-1.
- Bonewit-West K, Hunt SA, Applegate E. Today’s Medical Assistant: Clinical and Administrative Procedures. Elsevier Health Sciences; 2012. Page 571. ISBN 9781455701506.
- “Heroin”. Drugs.com. May 18, 2014. Archived from the original on October 19, 2016. Retrieved October 19, 2016.
- Rook EJ, van Ree JM, van den Brink W, Hillebrand MJ, Huitema AD, Hendriks VM, Beijnen JH. Pharmacokinetics and pharmacodynamics of high doses of pharmaceutically prepared heroin, by intravenous or by inhalation route in opioid-dependent patients. Basic & Clinical Pharmacology & Toxicology. January 2006;98(1):86–96. doi:10.1111/j.1742-7843.2006.pto_233.x. PMID 16433897.
- Riviello RJ. Manual of Forensic Emergency Medicine: A Guide for Clinicians. Sudbury, Mass.: Jones and Bartlett Publishers; 2010. Page 41. ISBN 978-0-7637-4462-5. Archived from the original on March 18, 2017. Retrieved August 29, 2017.
- “Diamorphine Hydrochloride Injection 30 mg – Summary of Product Characteristics”. electronic Medicines Compendium. ViroPharma Limited. September 24, 2013. Archived from the original on March 30, 2014. Retrieved March 30, 2014.
- Field J. The Textbook of Emergency Cardiovascular Care and CPR. Lippincott Williams & Wilkins; 2012. Page 447. ISBN 978-1-4698-0162-9. Archived from the original on September 10, 2017.
- Friedrichsdorf SJ, Postier A. Management of breakthrough pain in children with cancer. Journal of Pain Research. 2014;7:117–23. doi:10.2147/JPR.S58862. PMC 3953108. PMID 24639603.
- National Collaborating Centre for Cancer (UK). Opioids in Palliative Care: Safe and Effective Prescribing of Strong Opioids for Pain in Palliative Care of Adults. Cardiff (UK): National Collaborating Centre for Cancer (UK); May 2012. PMID 23285502.
- Uchtenhagen AA. Heroin maintenance treatment: from idea to research to practice (PDF). Drug and Alcohol Review. March 2011;30(2):130–7. doi:10.1111/j.1465-3362.2010.00266.x. PMID 21375613. Archived from the original (PDF) on August 28, 2021. Retrieved April 20, 2018.
- “Diamorphine”. SPS – Specialist Pharmacy Service. February 15, 2013.
- “DrugFacts—Heroin”. National Institute on Drug Abuse. October 2014. Archived from the original on October 19, 2016. Retrieved October 19, 2016.
- National Institutes on Drug Abuse. Research Report Series: Heroin (PDF). National Institutes on Drug Abuse; 2014. Page 1. Archived (PDF) from the original on December 30, 2016. “Highly pure heroin can be snorted or smoked and may be more appealing to new users because it eliminates the stigma associated with injection drug use… Impure heroin is usually dissolved, diluted, and injected into veins, muscles, or under the skin.”
- United Nations Office on Drugs and Crime. Statistical tables (PDF). World Drug Report 2016. Vienna, Austria; May 2016. Pages xii, 18, 32. ISBN 978-92-1-057862-2. Archived (PDF) from the original on August 9, 2016. Retrieved August 1, 2016.
- “Information sheet on opioid overdose”. WHO. August 2018. Archived from the original on April 21, 2019. Retrieved December 10, 2018.
- Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. (GBD 2015 Mortality and Causes of Death Collaborators). Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. October 2016;388(10053):1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903. PMID 27733281. “For GBD 2015, we have made major updates to the causes and risks of smoking, alcohol, drug use, and injuries to provide estimates for the year 2015.”