Contents
Summary
Methadone, available under trade names like Dolophine and Methadose, is a synthetic opioid analgesic utilized to manage moderate to severe pain and address opioid addiction. Its primary application is in the treatment and control of opioid addiction symptoms. While its subjective effects share similarities with other synthetic opioids like fentanyl, users often report a notably heightened sense of euphoria. Notably, the occurrence of cardiac arrhythmia, a potential side effect associated with the use of methadone, is relatively less frequent compared to dextropropropoxyphene use.
| Identifiers | |
|---|---|
| IUPAC name | |
| CAS Number | 76-99-3 |
|---|---|
| PubChem CID | 4095 |
| IUPHAR/BPS | 5458 |
| DrugBank | DB00333 |
| ChemSpider | 3953 |
| UNII | UC6VBE7V1Z |
| KEGG | D08195 |
| ChEBI | CHEBI:6807 |
| ChEMBL | ChEMBL651 |
| CompTox Dashboard (EPA) | DTXSID7023273 |
| ECHA InfoCard | 100.000.907 |
| Chemical and physical data | |
| Formula | C21H27NO |
| Molar mass | 309.453 g·mol−1 |
Chemistry
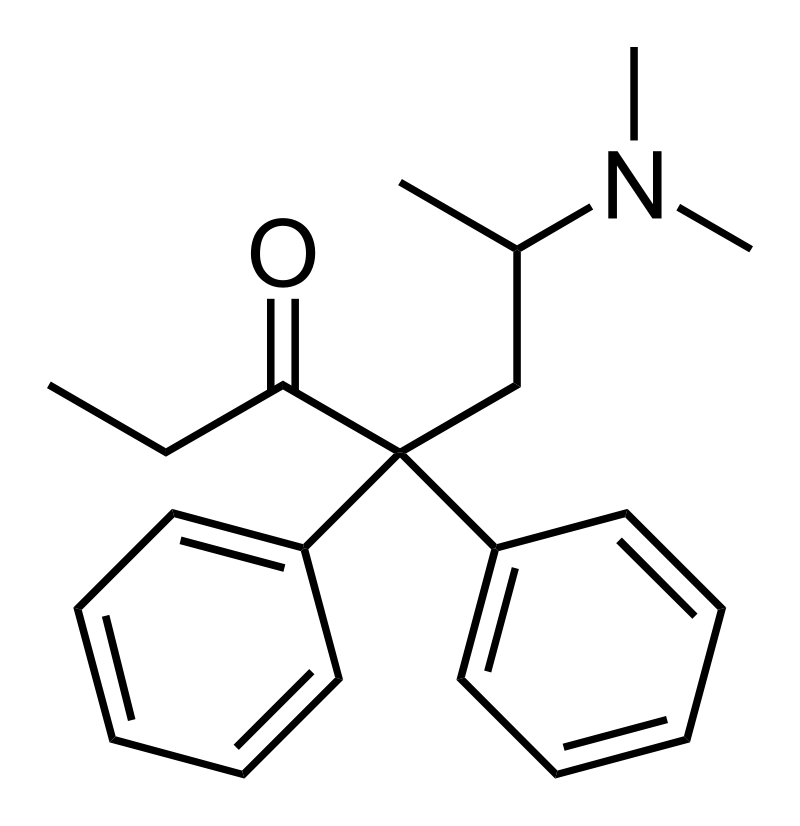
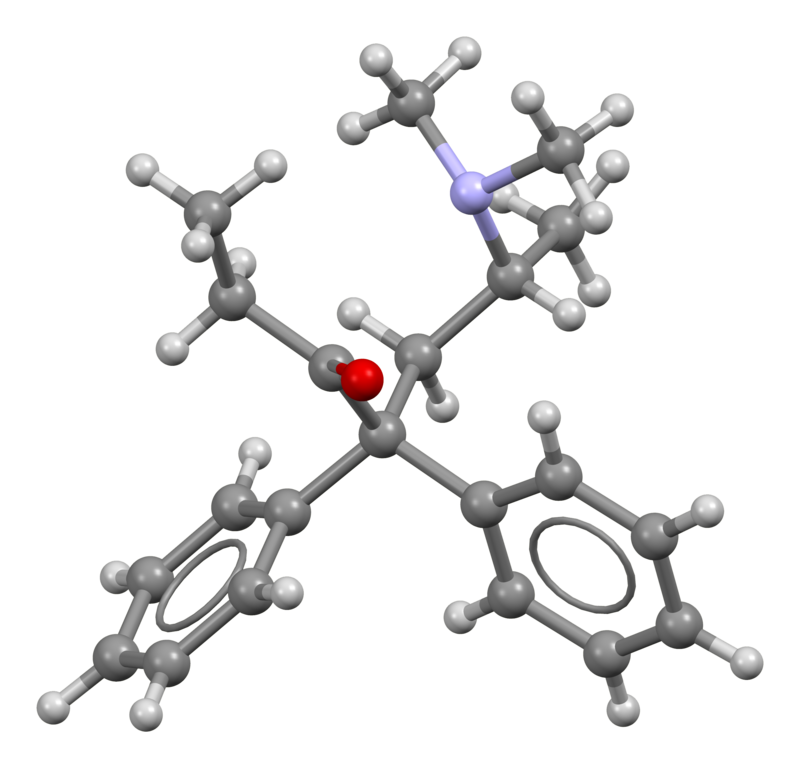
Methadone belongs to the diphenylpropylamine class of opioids, characterized by a structure featuring two phenyl rings attached to carbon R4 within the primary 2-oxo-6-dimethylaminoheptane chain. It exists in a racemic mixture comprising both dextromethadone and levomethadone. Structurally, it bears a resemblance to tapentadol and dextropropoxyphene.
Methadone, along with its primary metabolite known as 2-ethylidene-1,5-dimethyl-3,3-diphenylpyrrolidine (EDDP), is frequently quantified in urine as part of drug abuse testing protocols. It is also analyzed in plasma or serum to confirm potential poisoning cases in hospitalized individuals or in whole blood to aid forensic investigations related to traffic violations, criminal activities, or sudden deaths. Interpretation of results considers the individual’s history of methadone usage, as chronic users may develop tolerance levels that would hinder someone’s opioid-naive. Such individuals typically exhibit elevated baseline values for methadone and EDDP.
The protonated form of methadone adopts an extended conformation, whereas the free base form exhibits a more compact structure. Notably, there is an interaction between the tertiary amine and the carbonyl carbon of the ketone function (R3N ••• >C=O), which restricts the molecule’s conformational flexibility. Although the distance between these entities (measuring 291 pm via X-ray) is too extensive to denote an actual chemical bond, it signifies the initial path of attack of an amine on a carbonyl group, providing significant experimental evidence for the proposal of the Bürgi–Dunitz angle in carbonyl addition reactions.
Pharmacology
Opioids exert their effects by binding to and activating the μ-opioid receptor. This mechanism is possible because opioids structurally resemble endogenous endorphins naturally occurring in the body, which also act upon the μ-opioid receptor system. The structural similarity allows opioids to induce euphoria, alleviate pain, and provide anxiolytic effects. Endorphins play a vital role in pain reduction, inducing sleepiness and creating feelings of pleasure. These endorphins can be released in response to various stimuli, including pain, intense physical activity, orgasm, or general excitement. When opioids mimic these natural endorphins, it leads to the observed effects.
The bioavailability of orally administered methadone can vary widely, ranging from 40% to approximately 99%. Methadone undergoes metabolism through the cytochrome P450 system.
In contrast to most opioids, methadone exhibits weak serotonin reuptake inhibition and acts as a weak NMDA antagonist. Similar to dextropropoxyphene, methadone serves as a nicotinic acetylcholine receptor antagonist.
The metabolic half-life of methadone differs from its duration of action. Methadone has a metabolic half-life of 8 to 59 hours (around 24 hours for opioid-tolerant individuals and approximately 55 hours for opioid-naive individuals). In comparison, morphine has a half-life of 1 to 5 hours. The prolonged half-life of methadone allows it to exert respiratory depressant effects for an extended period in opioid-naive individuals.
Levomethadone (the L enantiomer) acts as a μ-opioid receptor agonist with higher intrinsic activity than morphine, albeit with lower affinity. Dextromethadone (the S enantiomer) does not affect opioid receptors but binds to the glutamatergic NMDA (N-methyl-D-aspartate) receptor and functions as an antagonist against glutamate. Methadone has demonstrated efficacy in reducing neuropathic pain, primarily through its NMDA receptor antagonism. Glutamate serves as the principal excitatory neurotransmitter in the central nervous system. Acting as an NMDA antagonist is one proposed mechanism by which methadone reduces opioid cravings and tolerance, making it especially effective in treating neuropathic pain.
Methadone also acts as a potent, noncompetitive antagonist of α3β4 neuronal nicotinic acetylcholine receptors in rat receptors, expressed in human embryonic kidney cell lines.
Binding affinities (Ki):
- Mu opioid agonist – 24.8 nM
- Kappa opioid agonist – 543 nM
- Delta opioid agonist – 1674 nM
Subjective effects
Important Note: The effects detailed below are based on the Subjective Effect Index (SEI), a research compilation drawing from anecdotal user reports and analyses by PsychonautWiki contributors. It is essential to approach these effects with a degree of skepticism.
Additionally, it’s crucial to understand that these effects may not manifest predictably or consistently. Higher doses are more likely to encompass the full spectrum of effects. Furthermore, it’s vital to be aware that adverse effects become more likely with higher doses and can include addiction, severe injury, or even death ☠.
Physical:
- Methadone generally induces a sense of euphoria, relaxation, anxiety reduction, and pain relief.
- Pain Relief
- Physical Euphoria: Methadone’s physical euphoria, while less intense compared to morphine or diacetylmorphine (heroin), is stronger than that of other synthetic opioids like tramadol. Users often describe it as an extreme sensation of profound physical comfort, warmth, love, and bliss.
- Itchiness
- Respiratory Depression: At low to moderate doses, methadone may mildly to moderately slow down breathing without causing significant impairment. However, at high doses or overdoses, it can lead to shortness of breath, abnormal breathing patterns, semi-consciousness, or unconsciousness. Severe overdoses can result in a coma or death without prompt medical attention.
- Constipation
- Cough Suppression
- Difficulty Urinating
- Nausea
- Sedation
- Pupil Constriction
- Decreased Libido
- Appetite Suppression
- Orgasm Suppression
- Abnormal Heartbeat: Methadone has the potential to prolong the QT interval, which can lead to a rare but potentially fatal side effect known as Torsades de Pointes. This abnormal heart rhythm can cause sudden cardiac death.
Cognitive:
- Cognitive Euphoria: Methadone’s cognitive euphoria is generally less intense than that of morphine or diacetylmorphine (heroin) but stronger than that of other synthetic opioids like tramadol. Users often describe it as a powerful and overwhelming feeling of emotional bliss, contentment, and happiness.
- Anxiety Suppression
- Compulsive Redosing
- Dream Potentiation
Toxicity
Note:
The information provided below offers insight into the potential risks associated with methadone use. Always exercise caution and prioritize harm-reduction practices when using this drug.
- Moderate Toxicity: Methadone carries a moderate level of toxicity relative to its dosage. Like all opioids, its long-term effects can vary and may include diminished libido, apathy, and memory loss.
- Dangerous Combinations: Methadone becomes potentially lethal when mixed with depressants like alcohol or benzodiazepines. It also has a broader range of substances that can be dangerous when combined with compared to other opioids. Importantly, methadone is known to lower the seizure threshold, so it should not be taken during benzodiazepine withdrawals as this can potentially trigger seizures.
- Harm Reduction: It is highly advisable to employ harm reduction practices when using methadone.
Tolerance and Addiction Potential
- Highly Addictive: Similar to other opioids, chronic methadone use can be highly addictive and carries a substantial potential for abuse. It can lead to psychological dependence in some users. Cravings and withdrawal symptoms may occur when a person abruptly discontinues its use.
- Tolerance Development: Prolonged and repeated methadone use often leads to tolerance, where users need progressively larger doses to achieve the same effects. The development of tolerance can vary for different effects, with the constipation-inducing effects developing particularly slowly.
- Cross-tolerance: Methadone exhibits cross-tolerance with all other opioids, meaning that after using methadone, the effects of other opioids will be diminished.
- Reduced Tolerance Risk: After a period of abstinence and relapse, the risk of fatal opioid overdoses significantly increases due to reduced tolerance. To mitigate this risk, it is safer to consume a fraction of one’s usual dosage when relapsing.
- Environmental Influence: Studies suggest that the environment in which a person uses a substance can impact opioid tolerance. For instance, in one study, rats with a history of heroin use were more likely to overdose when given the drug in an unfamiliar environment compared to a familiar one.
Dangerous Interactions
Warning: Combining certain substances with methadone can pose serious and even life-threatening risks. While the list below outlines some known dangerous interactions, it may not include all possibilities. Always conduct independent research to ensure the safety of combining two or more substances.
- Alcohol: Combining methadone and alcohol can potentiate the ataxia and sedation caused by each substance, potentially leading to loss of consciousness at high doses. Affected individuals should be placed in the recovery position to prevent aspiration from excess vomit. Memory blackouts are likely.
- Amphetamines: Stimulants like amphetamines increase respiration rate, allowing for higher opioid doses than usual. If the stimulant wears off first, the opioid can potentially overcome the user, leading to respiratory arrest.
- Benzodiazepines: Combining methadone with benzodiazepines can result in central nervous system and respiratory-depressant effects that are additive or synergistic, leading to rapid unconsciousness. While unconscious, there is a risk of vomit aspiration, and users may experience blackouts or memory loss.
- Cocaine: Cocaine, a stimulant, increases respiration rate and can permit higher opioid doses. However, if the stimulant wears off before the opioid, it can lead to respiratory arrest.
- DXM: DXM (dextromethorphan), often found in cough medications, is considered toxic when combined with opioids like methadone. It can lead to central nervous system depression, difficulty breathing, heart issues, and liver toxicity. Additionally, taking DXM may lower opioid tolerance slightly, potentially resulting in additional synergistic effects.
- GHB/GBL: These substances can strongly and unpredictably potentiate the effects of methadone, leading to rapid unconsciousness. While unconscious, there is a risk of vomit aspiration if the user is not placed in the recovery position.
- Ketamine: Both methadone and ketamine carry risks of vomiting and unconsciousness. Suppose a user becomes unconscious while under the influence; there is a severe risk of vomit aspiration if the recovery position is not applied.
- MAOIs: Combining certain monoamine oxidase inhibitors (MAOIs) with opioids can lead to rare, severe adverse reactions. These reactions may include agitation, headache, diaphoresis, hyperpyrexia, flushing, shivering, myoclonus, rigidity, tremor, diarrhea, hypertension, tachycardia, seizures, coma, and, in some cases, death.
- MXE: MXE can potentiate the effects of opioids like methadone but also increase the risk of respiratory depression and organ toxicity.
- Nitrous: Combining nitrous oxide with methadone can potentiate ataxia and sedation, potentially leading to unexpected loss of consciousness at high doses. While unconscious, there is a risk of vomit aspiration. Memory blackouts are common.
- PCP: PCP may reduce opioid tolerance, increasing the risk of overdose when combined with methadone.
- Tramadol: Combining tramadol with methadone can increase the risk of seizures. Tramadol itself is known to induce seizures, and its effects on the seizure threshold may be additive when combined with other opioids. Central nervous system and respiratory-depressant effects may also be additively or synergistically present.
- Grapefruit: Although not psychoactive itself, grapefruit can affect the metabolism of certain opioids, including methadone, by inhibiting the CYP3A4 enzyme. This can prolong the drug’s clearance from the body, potentially increasing its toxicity.
- Psychedelics: Methadone is known to lower the seizure threshold, and the use of psychedelics may act as a triggers for seizures in susceptible individuals.
Legal status
- Canada: Methadone is categorized as a Schedule I Controlled Substance.
- Germany: Methadone is classified as a controlled substance under Anlage III of the BtMG. It can only be prescribed using a narcotic prescription form.
- Russia: Methadone is designated as a Schedule I controlled substance.
- Switzerland: Methadone is recognized as a controlled substance specifically listed under Verzeichnis A. Medicinal use is permitted.
- United Kingdom: In the United Kingdom, Methadone is classified as a Class A drug and is listed under Schedule 2.
- United States: Methadone is classified as a Schedule II Controlled Substance in the United States.
FAQ
- What is Methadone?
- Methadone is a synthetic opioid medication used primarily to treat pain and opioid addiction. It’s part of a class of drugs known as opioids.
- How is Methadone typically used?
- Methadone is usually administered orally, either as a tablet, liquid, or dispersible powder. It’s commonly used in opioid addiction treatment programs and for managing chronic pain.
- What is the purpose of Methadone in opioid addiction treatment?
- Methadone is used to reduce cravings and withdrawal symptoms in individuals addicted to opioids like heroin or prescription painkillers. It helps them stabilize their lives and engage in treatment.
- Is Methadone safe to use for pain management?
- Yes, when prescribed and used as directed by a healthcare professional, Methadone can be a safe and effective pain management option. However, it must be used cautiously due to its potential for addiction.
- What are the potential side effects of Methadone?
- Common side effects may include drowsiness, constipation, nausea, and sweating. More severe side effects can occur, so it’s essential to follow your doctor’s guidance closely.
- Is Methadone addictive?
- Yes, Methadone has a potential for addiction, especially when misused or taken in higher doses than prescribed. It should only be used under medical supervision.
- Can Methadone overdose occur?
- Yes, like other opioids, Methadone can lead to overdose if taken in excessive amounts. Overdose symptoms may include difficulty breathing, extreme drowsiness, and unconsciousness, which can be life-threatening.
- How is Methadone different from other opioids like heroin or oxycodone?
- Methadone is a long-acting opioid, which means its effects last longer than many other opioids. This property makes it suitable for addiction treatment. It also has a milder euphoric effect compared to drugs like heroin.
- Can Methadone be used during pregnancy?
- Methadone treatment during pregnancy is sometimes recommended for pregnant individuals with opioid addiction. However, it should be closely monitored by healthcare professionals to minimize risks to both the mother and baby.
- Is it safe to drink alcohol while taking Methadone?
- It’s generally not safe to consume alcohol while taking Methadone, as both substances can depress the central nervous system, potentially leading to dangerous interactions and respiratory depression.
- How can I stop using Methadone safely?
- If you’re on Methadone maintenance treatment for opioid addiction, it’s essential to work with a healthcare provider to taper off the medication gradually. Stopping abruptly can lead to withdrawal symptoms and relapse.
- Is Methadone legal in my country?
- Methadone’s legal status varies by country. It’s classified as a controlled substance in many places, so you should check your local regulations and consult a healthcare professional for guidance.
References
- Pharmacokinetics and Toxicology: Understanding the way drugs and chemicals interact with the body is crucial. Methadone’s disposition in the human body has been extensively studied.
- Chemical Conformation and Pharmacology: The way Methadone is structured and how it interacts with receptors can impact its effects.
- Methadone Overdose Prevention: Methadone overdoses can be dangerous, and measures to keep patients safe have been explored.
- Opioids in Cancer Pain: Methadone is sometimes used in the management of cancer pain.
- Nicotinic Receptor Function: Understanding how Methadone affects nicotinic receptors is important.
- Dihydrocodeine Affinities: Information on dihydrocodeine and its receptor binding affinities.
- Torsade de Pointes Risk: Methadone use has been associated with a specific type of heart rhythm abnormality.
- Environmental Cues in Heroin Overdose: Factors contributing to heroin overdose, including environmental cues, have been studied.
- Grapefruit Juice Interaction: Exploring the interactions between grapefruit juice and Methadone.
- Monoamine Oxidase Inhibitors: The interaction between monoamine oxidase inhibitors and opioid analgesics, including Methadone.
- Consolidated Federal Laws of Canada: Information on the legal status of Methadone in Canada.
- Anlage III BtMG: Methadone’s controlled status in Germany.
- Russian Government Resolution: Regulatory details regarding Methadone in Russia.
- Swiss Federal Chancellery: Information on Methadone’s status in Switzerland.
- Misuse of Drugs Legislation: A list of commonly controlled drugs under drug misuse laws.
- DEA Controlled Substances: Information on Methadone’s classification in the United States.