Amphetamine research chemical sellers are increasingly prevalent online, offering various designer drugs purportedly for research purposes. However, this burgeoning industry raises numerous concerns that merit a critical review.
First and foremost, the credibility of these sellers could be better at best. The online nature of their operations makes it difficult to verify the authenticity of their products or the legitimacy of their claims. This lack of transparency and regulation poses a significant risk to potential buyers who may unknowingly purchase impure or even dangerous substances masquerading as research chemicals.
Moreover, the ethical implications of selling amphetamines and other potentially harmful compounds online cannot be understated. While some may argue that these substances are intended for scientific research, it is evident that many customers are buying them for recreational use. These sellers, knowingly or unknowingly, may contribute to substance abuse problems and societal health hazards.
The need for proper quality control and safety measures is another pressing issue. Unlike pharmaceutical-grade amphetamines, which undergo rigorous testing and quality control, research chemicals from online vendors often lack such assurance. Buyers are left to their own devices when assessing purity and dosage, which can have dire consequences for their health and safety.
Furthermore, selling amphetamines as research chemicals skirts the legal boundaries in many jurisdictions, exploiting regulatory gaps for financial gain. This raises concerns about the moral responsibility of these vendors and their commitment to public well-being.
Contents
- 1 Summary
- 2 History and culture
- 3 Chemistry
- 4 Pharmacology
- 5 Subjective effects
- 6 Toxicity
- 7 Reagent results
- 8 Legal status
- 9 FAQ
- 9.1 1. What is amphetamine?
- 9.2 2. What are some common street names for amphetamine?
- 9.3 3. How does amphetamine work?
- 9.4 4. What are the effects of amphetamine use?
- 9.5 5. Is amphetamine addictive?
- 9.6 6. What are the potential health risks associated with amphetamine use?
- 9.7 7. How is amphetamine-regulated legally?
- 9.8 8. Can amphetamine be used safely for medical purposes?
- 9.9 9. What is the recommended approach to harm reduction when using amphetamine?
- 9.10 10. Is amphetamine use associated with any long-term effects on the brain?
- 10 References
Summary
Amphetamine, also known as alpha-methylphenethylamine or by street names like “speed” and recognized under brand names such as Adderall and Dexedrine, falls into the classical stimulant category within the phenethylamine class of substances. This compound is the precursor to a diverse group of substituted amphetamines, encompassing drugs like methamphetamine, MDMA, cathinone, and bupropion. The central mechanism of action revolves around its ability to facilitate the release of neurotransmitters like dopamine and norepinephrine.
This chemical entity was initially synthesized in 1887, but its psychostimulant properties remained undiscovered until 1929. During the 1930s, it was marketed over the counter as “Benzedrine,” primarily as a decongestant. Over time, it found applications in treating various conditions, including alcohol hangovers, narcolepsy, depression, and obesity. However, due to mounting concerns related to addiction and misuse, it was eventually categorized as a controlled substance under the United Nations’ 1971 “Convention on Psychotropic Substances.”
In contemporary times, amphetamine is a prescription medication primarily used to address conditions such as attention deficit hyperactivity disorder (ADHD), narcolepsy, and obesity. Concurrently, it has gained notoriety as an illicit substance, frequently employed for performance enhancement and recreational purposes.
Subjective effects encompass heightened alertness, improved focus, enhanced motivation, increased libido, appetite suppression, and euphoria. It can also be administered orally via insufflation, injection, or rectal administration. Lower doses improve concentration and productivity, while higher doses often lead to increased sociability, heightened sexual desire, and intensified euphoric sensations.
Amphetamine carries a significant risk of abuse, especially with chronic use involving high doses and repeated administration. This pattern of service can result in compulsive redosing, escalating tolerance, and psychological dependence. Furthermore, abuse has been linked to various health complications, particularly cardiovascular issues like elevated blood pressure and an increased risk of stroke.
It is strongly recommended to practice harm reduction measures when considering the use of this substance.
| Identifiers | |
|---|---|
| show IUPAC name | |
| CAS Number | 300-62-9 |
| PubChem CID | 3007 |
| IUPHAR/BPS | 4804 |
| DrugBank | DB00182 |
| ChemSpider | 13852819 |
| UNII | CK833KGX7E |
| KEGG | D07445 |
| ChEBI | CHEBI:2679 |
| ChEMBL | ChEMBL405 |
| NIAID ChemDB | 018564 |
| CompTox Dashboard (EPA) | DTXSID4022600 |
| ECHA InfoCard | 100.005.543 |
| Chemical and physical data | |
| Formula | C9H13N |
| Molar mass | 135.210 g·mol−1 |
History and culture
Amphetamine’s origins trace back to its synthesis in Germany in 1887 by the Romanian chemist Lazăr Edeleanu, who initially dubbed phenylisopropylamine. However, it wasn’t until 1927 that its stimulating properties came to light when Gordon Alles independently re-synthesised it, leading to the discovery of its sympathomimetic effects.
In the latter part of 1933, Smith, Kline and French introduced amphetamine as a decongestant inhaler, branding it as Benzedrine. Three years later, Benzedrine sulfate debuted and found application in treating various medical conditions, including narcolepsy, obesity, low blood pressure, reduced libido, and chronic pain.
The landscape changed significantly during World War II, with Allied and Axis forces extensively employing amphetamine and methamphetamine for their stimulant and performance-enhancing attributes. However, as the addictive potential of these substances became evident, governments began imposing stringent controls on their distribution and sale.
Amphetamine continues to be illegally synthesized and distributed on the black market, primarily in European countries. Among European Union (EU) member states, illicit amphetamine or methamphetamine use was reported by 1.2 million young adults in 2013. In 2012, EU member states confiscated approximately 5.9 metric tons of illegal amphetamine, with the “street price” of illicit amphetamine within the EU ranging from €6 to €38 per gram during the same period.
Beyond Europe, the illicit amphetamine market remains considerably smaller than the markets for methamphetamine and MDMA.
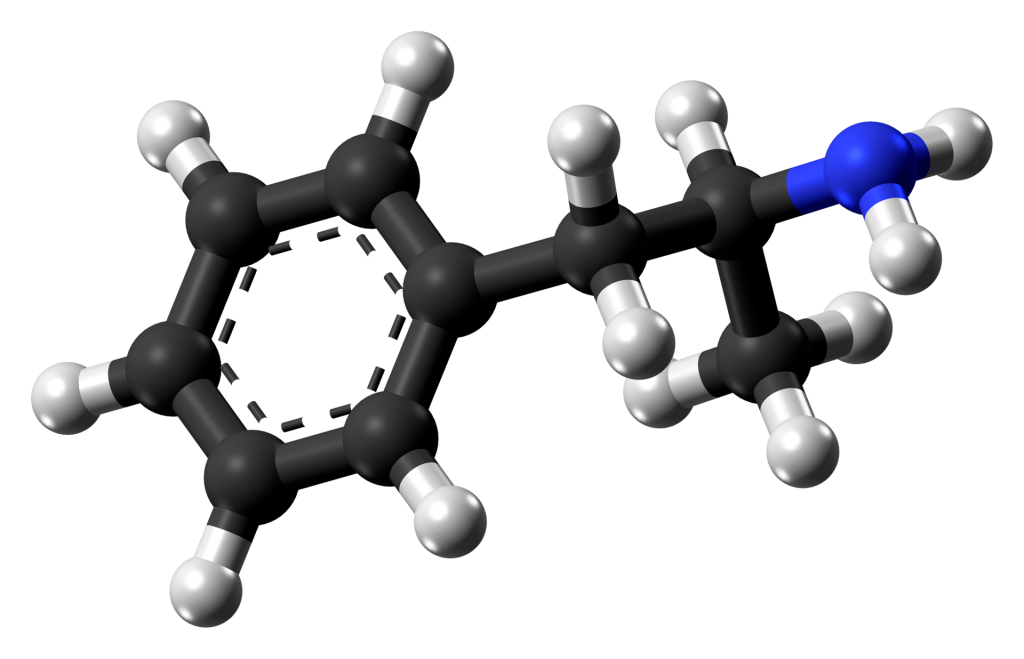
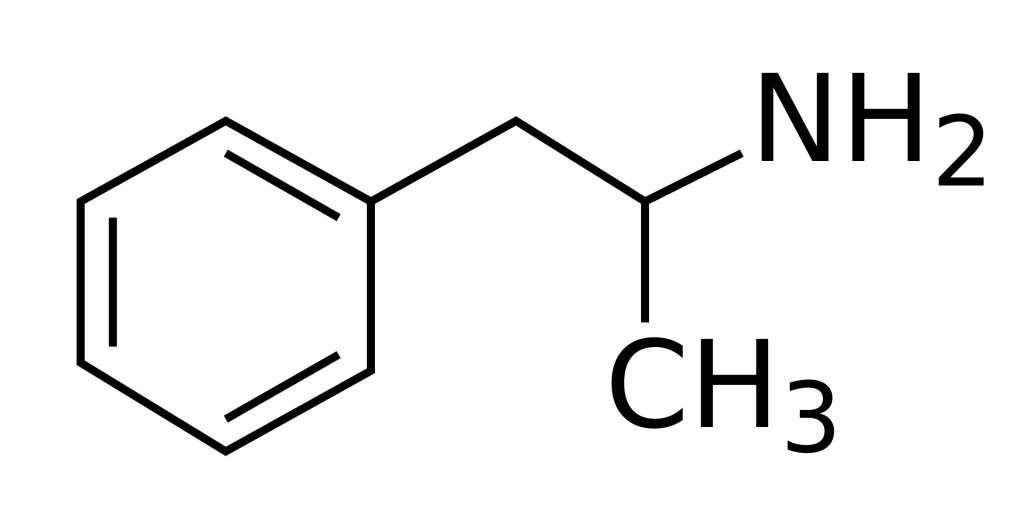
Chemistry
Amphetamine, also called alpha-methylphenethylamine, is a synthetic compound belonging to the phenethylamine family. Its chemical structure comprises a phenethylamine backbone featuring a phenyl ring connected to an amino (NH2) group through an ethyl chain, along with an additional methyl group substitution at the Rα position. The term ‘amphetamine’ is derived from its original name, αlphamethylphenethylamine, reflecting its chemical composition.
Amphetamine is the precursor for a diverse group of substances known as substituted amphetamines. This group encompasses many compounds, including bupropion, phenmetrazine, methamphetamine, MDMA, and the DOx series.
At standard room temperature, the pure freebase form of amphetamine manifests as a mobile, colourless, and volatile liquid characterized by a distinct and potent amine odour accompanied by an acrid, burning taste.
Amphetamine exhibits chirality, meaning it exists in two distinct enantiomer forms:
- L-amphetamine (levamfetamine): This is the ‘left-handed’ enantiomer of amphetamine.
- D-amphetamine (dextroamphetamine): This is the ‘right-handed’ enantiomer of amphetamine.
Various formulations of amphetamine, including Adderall, comprise a mixture of these enantiomers in a 3:1 ratio of d to l. Achieving this ratio involves combining one part racemic amphetamine with one part d-amphetamine, a commonly employed practice in pharmaceutical preparations.
Pharmacology
Amphetamine exerts its behavioural effects by augmenting the signalling activity of the neurotransmitters norepinephrine and dopamine within the brain’s reward and executive function pathways. The reinforcing and motivational impacts of amphetamine primarily stem from its ability to enhance dopaminergic activity in the mesolimbic path.
The euphoric and locomotor-stimulating consequences of amphetamine hinge on the extent and rapidity with which it elevates synaptic concentrations of dopamine and norepinephrine in the striatum.
Amphetamine acts as a potent full agonist of the trace amine-associated receptor 1 (TAAR1) and interacts with the vesicular monoamine transporter 2 (VMAT2). This dual action on TAAR1 and VMAT2 results in heightened levels of dopamine and norepinephrine in the synapses, thus promoting neuronal activity.
Notably, dextroamphetamine displays greater potency as a TAAR1 agonist than levoamphetamine. Consequently, dextroamphetamine induces more pronounced central nervous system stimulation, approximately three to four times greater than levoamphetamine. However, levoamphetamine does exhibit slightly stronger cardiovascular and peripheral effects.
Regarding its bioavailability, the precise figure remains uncertain. Still, oral administration is believed to achieve an absorption rate of over 75%, even higher when administered via injection or intranasal routes. PH levels may also influence the absorption and excretion processes. The basic form of amphetamine is more readily absorbed in the intestine and less efficiently eliminated by the kidneys, potentially leading to an extended half-life. Removal from the body primarily occurs through renal excretion, with a minor portion being metabolized by hepatic enzymes.

Subjective effects
Disclaimer: The ensuing effects are drawn from anecdotal user reports and contributors’ insights to the Subjective Effect Index (SEI), a body of open research literature. These observations should be approached with a measure of scepticism.
It’s essential to note that these effects may not manifest uniformly or predictably, with higher doses being more likely to encompass the full range of outcomes. Additionally, it’s crucial to be aware that elevated amounts can heighten the probability of adverse effects, including addiction, severe harm, or even fatality ☠.
Physical:
- Stimulation: Amphetamine is often highly energizing and stimulating, prompting physical activities such as dancing, socializing, running, or cleaning. This stimulation can become forceful, making it challenging to remain still, particularly at higher dosages. Notably, it may lead to jaw clenching, involuntary bodily tremors, and vibrations, resulting in pronounced shaking and impaired fine motor control. Fatigue and exhaustion may set in during the experience’s descent.
- Spontaneous bodily sensations: The “body high” linked to amphetamine is characterized by a moderate, euphoric tingling sensation enveloping the entire body. This sensation persists and intensifies as the onset progresses, reaching its zenith during the peak.
- Physical euphoria
- Abnormal heartbeat
- Increased heart rate
- Increased blood pressure: Some reports suggest an increase in systolic blood pressure by approximately 30mmHg and diastolic blood pressure by 20mmHg in naive users taking 40mg d-AMP.
- Appetite suppression
- Bronchodilation
- Dehydration
- Dry mouth
- Frequent urination
- Difficulty urinating
- Increased bodily temperature
- Increased perspiration
- Mania: Amphetamine may induce sensation in individuals with a genetic predisposition, such as those on the bipolar disorder or schizophrenia spectrum. Higher doses and sleep deprivation appear to heighten this risk.
- Nausea: Eating before dosing and during the experience may help mitigate nausea.
- Pupil dilation: This effect becomes noticeable mainly at common to high doses and in low-light conditions, being more prominent during the comedown.
- Reflex syncope
- Stamina enhancement
- Teeth grinding: Although teeth grinding may occur at higher doses, it is generally less intense than that associated with MDMA.
- Temporary erectile dysfunction
- Vasoconstriction: Amphetamine’s use constricts blood vessels, potentially causing sensations of tingling, pain, coldness, numbness, paleness, or changes in skin colour, particularly in the fingers and toes.
Visual:
- Distortions
- Drifting: This effect tends to be subtle and barely noticeable, typically occurring at higher dosages or in conjunction with cannabis. It usually falls within level 1-2 drifting.
- Brightness alteration: Amphetamine can make spaces appear brighter due to its pupil-dilating effects.
- Tracers: Imperceptible at low doses, tracers become more pronounced with larger quantities, especially when sleep deprivation is a contributing factor.
Hallucinatory states:
- Transformations: Transformations are exceedingly rare and typically manifest with high doses, during the comedown, or after prolonged wakefulness. They are generally mild when they do occur.
- Geometry: This effect, reported by some amphetamine users and related substances, is more common at heavier doses when attempting to sleep. It is simplistic, algorithmic, synthetic, dimly lit, multicoloured, glossy, sharp-edged, zoomed out, smooth, angular, immersive, and progressive. Typically, it starts at level 3 but may progress to levels 4 and 5 when combined with substances like cannabis or DXM.
Cognitive:
- Analysis enhancement: This effect is more consistent and prevalent than other common stimulants.
- Cognitive euphoria
- Compulsive redosing: This behavioural effect is typically less pronounced than cocaine or when amphetamine is insufflated rather than taken orally.
- Ego inflation
- Emotion suppression: Most intense at light and ordinary doses or with frequent usage, this effect is more commonly reported in medical contexts than in recreational ones.
- Focus enhancement: Most effective at low to moderate doses, as higher doses may impair concentration or lead to excessive physical activity and restlessness.
- Increased libido: While amphetamine can heighten feelings of sexual desire, constricted blood vessels may hinder achieving or maintaining an erection.
- Increased music appreciation
- Irritability: More likely to occur at higher doses and during the comedown.
- Memory enhancement
- Motivation enhancement: Anecdotal reports suggest this aspect may be more pronounced when the levoamphetamine enantiomer is present in the substance, as in racemic amphetamine or mixtures like Adderall.
- Psychosis: This effect occurs in predisposed individuals with chronic, high-frequency use or due to sleep deprivation. Repeated administration of threshold/very low dosages may also be associated with this effect, possibly related to the “dopamine hypersensitivity” hypothesis. However, this topic remains somewhat controversial and speculative.
- Suggestibility suppression
- Thought acceleration
- Thought organization
- Time distortion is the perception of time speeding up and passing much more quickly than usual due to elevated dopamine levels.
- Wakefulness: Generally considered less intense than with methamphetamine but more potent than with cocaine.
After:
- Anxiety: Anxiety can reach severe levels during the comedown for some users.
- Appetite suppression
- Cognitive fatigue
- Depression
- Increased heart rate: Notably, heart rate peaks around 10 hours after administration, much later than the peak in blood concentration and most subjective effects.
- Irritability
- Restless legs
- Sleep paralysis: Some users report sleep paralysis after consuming amphetamine.
- Dream suppression
- Thought deceleration
- Wakefulness: Insomnia following repeated amphetamine doses may persist for more than a day in some users.
- Motivation suppression: This effect, ranging from mild demotivation to extreme disinterest, is more prominent at ordinary and heavy doses.
Toxicity
As of March 2014, no concrete evidence suggests that amphetamine directly induces neurotoxicity in humans. Nonetheless, high doses of amphetamine can potentially lead to indirect neurotoxicity due to increased oxidative stress resulting from reactive oxygen species and the autoxidation of dopamine.
In rodents and primates, sufficiently elevated doses of amphetamine have been observed to cause damage to dopamine neurons, characterized by diminished transporter and receptor functionality. Animal models illustrating neurotoxicity resulting from high-dose amphetamine exposure indicate that hyperpyrexia (core body temperature ≥ 40 °C) is necessary for the development of amphetamine-induced neurotoxicity.
Melatonin has demonstrated the ability to prevent (when used 30 minutes or more before dosing) and reverse amphetamine-induced neurotoxicity concerning TH-pSer40 and calpastatin levels in the Substantia Nigra of rats.
It is strongly advised to employ harm reduction practices when using this substance.
Lethal Dosage The LD50 (the dosage required to cause death in 50% of test subjects) of amphetamine in rats has been estimated to range from approximately 15 mg to 180 mg per kilogram, depending on the study. No formal human studies have been conducted to determine the exact toxic dosage.
Dependence and Abuse Potential Amphetamine carries a high potential for abuse and can lead to psychological support with chronic use.
Once dependence has developed, users may experience cravings and withdrawal effects if the substance is abruptly discontinued. Withdrawal symptoms can include paranoia, depression, potentiation of dreams, anxiety, itching, mood swings, irritability, fatigue, insomnia, and an intense desire for more amphetamine or other stimulants.
Addiction is a significant risk associated with chronic or heavy recreational amphetamine use but is unlikely to arise from typical medical use.
Tolerance to many of the effects of amphetamine typically develops with prolonged and repeated use. This necessitates the administration of increasingly larger doses to achieve the same impact. After a single administration, tolerance takes about 3 – 7 days to reduce by half and 1 – 2 weeks to return to baseline (in the absence of further consumption). Amphetamine demonstrates cross-tolerance with all dopaminergic stimulants, meaning that after using amphetamine, most stimulants will have a reduced effect.
Psychosis Severe amphetamine overdose can lead to stimulant psychosis, characterized by various symptoms such as paranoia, hallucinations, and delusions. A review of the treatment of amphetamine abuse-induced psychosis indicates that about 5–15% of users fail to recover fully. The same study states that antipsychotic medications are effective in resolving the symptoms of acute amphetamine psychosis.[47] Psychosis rarely arises from therapeutic use.
Dangerous Interactions Warning: The combination of certain substances can suddenly become dangerous and even life-threatening. The following list highlights some known dangerous interactions, although it may not encompass all potential risks. Always conduct independent research (e.g., using search engines like Google or DuckDuckGo or consulting PubMed) to confirm the safety of combining two or more substances.
- Alcohol: Consuming alcohol with stimulants is considered risky because it diminishes the sedative effects of alcohol that the body uses to gauge drunkenness. This often leads to excessive drinking with reduced inhibitions, increasing the risk of liver damage and dehydration. The stimulating effects of stimulants may also allow individuals to consume more alcohol than they would typically tolerate, raising the risk.
- GHB/GBL: Stimulants increase respiration rate, potentially allowing for higher doses of sedatives. If the stimulant’s effects wear off before the depressant’s, GHB/GBL may overcome the user, leading to respiratory arrest.
- Opioids: Stimulants boost respiration rate, enabling a higher dose of opiates. If the stimulant effects dissipate before the opioid effects, the opiates may overwhelm the user, leading to respiratory arrest.
- Cocaine: Combining cocaine with amphetamine may result in cardiac effects due to the interaction of the two substances. Cocaine’s rewarding effects are mediated by DAT inhibition and increased dopamine exocytosis. Amphetamine, on the other hand, reverses DAT direction and vesicular transports within the cell through a pH-mediated mechanism, disrupting regular dopamine release via exocytosis. This interaction can lead to cardiac issues, especially when combined with amphetamines’ tendency to cause hypertension.
- Cannabis: Stimulants can elevate anxiety levels and the risk of thought loops and paranoia, potentially leading to negative experiences when combined with cannabis.
- Caffeine: Combining these two stimulants is generally considered unnecessary and may place additional strain on the heart while potentially causing anxiety and physical discomfort.
- Tramadol: Both stimulants and tramadol can raise heart rate and, in extreme cases, lead to panic attacks, possibly causing more severe heart issues.
- DXM: Both substances elevate heart rate and, in extreme cases, can cause panic attacks, potentially resulting in more severe heart problems.
- Ketamine: Combining amphetamine and ketamine may lead to psychoses resembling schizophrenia, although this may not necessarily be worse than the psychoses produced by each substance individually. This interaction can result from amphetamine’s capacity to attenuate the disruption of working memory caused by ketamine.
- PCP: The combination can increase the risk of tachycardia, hypertension, and manic states.
- Methoxetamine: Combining these substances can elevate the risk of tachycardia, hypertension, and manic states.
- Psychedelics (e.g., LSD, mescaline, psilocybin): Combining stimulants with psychedelics may heighten the risk of anxiety, paranoia, and thought loops.
- 25x-NBOMe: Both amphetamines and NBOMes provide considerable stimulation, which, when combined, can lead to tachycardia, hypertension, vasoconstriction, and, in extreme cases, heart failure. The anxiogenic and focusing effects of stimulants can also exacerbate unpleasant thought loops. NBOMes are known to cause seizures, and motivations can increase this risk.
- 2C-T-x and 5-MeO-xxT: Suspected to have mild MAOI properties, these substances may increase the risk of hypertensive crisis when combined with amphetamines.
- DOx and aMT: aMT possesses MAOI properties that may interact unfavourably with amphetamines.
- MAOIs: MAO-B inhibitors can unpredictably enhance the potency and duration of phenethylamines. MAO-A inhibitors, when combined with amphetamines, can lead to hypertensive crises.
Reagent results
Exposing compounds to the reagents gives a colour change which is indicative of the compound under test.
| Marquis | Mecke | Mandelin | Liebermann | Froehde | Robadope |
|---|---|---|---|---|---|
| Orange – red | No reaction | slow (dark) green | Orange – red | No reaction | Pink |
| Ehrlich | Hofmann | Simon’s | Scott | Folin | |
| No reaction | No reaction | No reaction | No reaction | Light orange | |
Legal status
Internationally, amphetamine is classified as a Schedule II controlled substance under the United Nations 1971 Convention on Psychotropic Substances.
Here is the classification of amphetamine in various countries:
- Australia: Amphetamine is categorized as a Schedule 8 controlled substance.
- Austria: Possession, production, and sale of amphetamine are illegal under the SMG (Suchtmittelgesetz Österreich).[citation needed]
- Brazil: Amphetamine is considered a Class A3 psychoactive substance
- Canada: Amphetamine is listed as a Schedule I drug in Canada.
- Germany: Amphetamine was incorporated into the Opiumgesetz (Opium Act) in 1941. According to the Narcotics Act reform of 1981, it falls under Anlage III BtMG (Narcotics Act, Schedule III) and can only be prescribed on a narcotic prescription form.
- Japan: Amphetamine is prohibited for any medical use in Japan.
- Luxembourg: Amphetamine is prohibited for recreational use in Luxembourg.
- The Netherlands: Amphetamine is classified as a List I controlled substance.
- New Zealand: Amphetamine is designated as a Class B controlled substance.
- South Korea: Amphetamine is prohibited, even for medical use, in South Korea.
- Sweden: Amphetamine is categorized as a drug by the United Nations and is listed in List P II of the 1971 Psychotropic Convention and List II in Sweden.
- Switzerland: Amphetamine is considered a controlled substance, named explicitly under Verzeichnis A. Medicinal use is permitted.
- Thailand: Amphetamine is classified as a category one narcotic under the Thai Narcotic Act 2012.
- United Kingdom: Amphetamine is classified as a Class B drug in the United Kingdom.
- United States: Amphetamine is recognized as a Schedule II controlled substance in the United States.
FAQ
1. What is amphetamine?
Amphetamine is a synthetic stimulant substance that belongs to the phenethylamine class. It is known for its stimulating effects on the central nervous system. It is commonly used to treat attention deficit hyperactivity disorder (ADHD), narcolepsy, and obesity.
2. What are some common street names for amphetamine?
Amphetamine is known by various street names, including “speed,” “uppers,” “whizz,” and “dexies.” It can also be found in prescription medications under brand names like Adderall and Dexedrine.
3. How does amphetamine work?
Amphetamine primarily works by increasing the activity of neurotransmitters, particularly dopamine and norepinephrine, in the brain’s reward and executive function pathways. This results in increased alertness, focus, and energy.
4. What are the effects of amphetamine use?
The results of amphetamine use can include increased energy, alertness, focus, and sociability. It can also lead to appetite suppression, increased heart rate, and elevated blood pressure. At higher doses, amphetamine use may result in euphoria, increased libido, and even hallucinations.
5. Is amphetamine addictive?
Yes, amphetamine has a high potential for abuse and can lead to psychological dependence with chronic use. Abrupt discontinuation of amphetamine can result in withdrawal symptoms such as depression, fatigue, and cravings.
6. What are the potential health risks associated with amphetamine use?
Amphetamine use can be related to various health risks, including cardiovascular issues like high blood pressure and an increased risk of stroke. Chronic use may lead to compulsive redosing, escalating tolerance, and psychological dependence.
7. How is amphetamine-regulated legally?
The legal status of amphetamine varies by country. It is classified as a controlled substance and tightly regulated in many places. In the United States, for example, it is classified as a Schedule II controlled substance, indicating a high potential for abuse.
8. Can amphetamine be used safely for medical purposes?
When prescribed and used as directed by a healthcare professional, amphetamine can be safe and effective for treating conditions like ADHD and narcolepsy. However, it should only be used under medical supervision to minimize the risk of abuse and adverse effects.
9. What is the recommended approach to harm reduction when using amphetamine?
If using amphetamine, it is crucial to practice harm reduction. This includes taking the prescribed dose as directed by a healthcare provider, avoiding excessive or recreational use, staying hydrated, and getting regular check-ups to monitor your health.
10. Is amphetamine use associated with any long-term effects on the brain?
While amphetamine use can lead to changes in brain chemistry, the long-term impact on the brain remains a research subject. Chronic, high-dose service may have more significant and lasting effects on cognitive function and mental health.
Remember that amphetamine use can have serious consequences, and you must consult a healthcare professional if you have any questions or concerns about its use or effects on your health.
References
- Kish, S. J. (17 June 2008). “Pharmacologic mechanisms of crystal meth”. Canadian Medical Association Journal. 178 (13): 1679–1682. doi:10.1503/cmaj.071675. ISSN 0820-3946.
- Heal, D. J., Smith, S. L., Gosden, J., Nutt, D. J. (June 2013). “Amphetamine, past and present – a pharmacological and clinical perspective”. Journal of Psychopharmacology. 27 (6): 479–496. doi:10.1177/0269881113482532. ISSN 0269-8811.
- Rasmussen, N. (21 February 2006). “Making the First Anti-Depressant: Amphetamine in American Medicine, 1929-1950”. Journal of the History of Medicine and Allied Sciences. 61 (3): 288–323. doi:10.1093/jhmas/jrj039. ISSN 0022-5045.
- Angrist, B., Sudilovsky, A. (1978). “Stimulants”. In Iversen, L. L., Iversen, S. D., Snyder, S. H. Central Nervous System Stimulants: Historical Aspects and Clinical Effects. Handbook of Psychopharmacology. Springer US. pp. 99–165. doi:10.1007/978-1-4757-0510-2_3. ISBN 9781475705102.
- Hodgkins, P., Shaw, M., McCarthy, S., Sallee, F. R. (1 March 2012). “The pharmacology and clinical outcomes of amphetamines to treat ADHD: does composition matter?”. CNS drugs. 26 (3): 245–268. doi:10.2165/11599630-000000000-00000. ISSN 1179-1934.
- Billiard, M. (June 2008). “Narcolepsy: current treatment options and future approaches”. Neuropsychiatric Disease and Treatment. 4 (3): 557–566. ISSN 1176-6328.
- Westover, A. N., McBride, S., Haley, R. W. (1 April 2007). “Stroke in Young Adults Who Abuse Amphetamines or Cocaine: A Population-Based Study of Hospitalized Patients”. Archives of General Psychiatry. 64 (4): 495. doi:10.1001/archpsyc.64.4.495. ISSN 0003-990X.
- Edeleano, L. (January 1887). “Ueber einige Derivate der Phenylmethacrylsäure und der Phenylisobuttersäure”. Berichte der deutschen chemischen Gesellschaft. 20 (1): 616–622. doi:10.1002/cber.188702001142. ISSN 0365-9496.
- Sulzer, D., Sonders, M. S., Poulsen, N. W., Galli, A. (April 2005). “Mechanisms of neurotransmitter release by amphetamines: A review”. Progress in Neurobiology. 75 (6): 406–433. doi:10.1016/j.pneurobio.2005.04.003. ISSN 0301-0082.
- Bett, W. R. (1 August 1946). “Benzedrine Sulphate in Clinical Medicine”. Postgraduate Medical Journal. 22 (250): 205–218. doi:10.1136/pgmj.22.250.205. ISSN 0032-5473.
- Rasmussen, N. (September 2011). “Medical Science and the Military: The Allies’ Use of Amphetamine during World War II”. The Journal of Interdisciplinary History. 42 (2): 205–233. doi:10.1162/JINH_a_00212. ISSN 0022-1953.
- Defalque, R. J., Wright, A. J. (April 2011). “Methamphetamine for Hitler’s Germany: 1937 to 1945”. Bulletin of Anesthesia History. 29 (2): 21–32. doi:10.1016/S1522-8649(11)50016-2. ISSN 1522-8649.
- “Historical overview of methamphetamine”. Vermont Department of Health. Government of Vermont. Archived from the original on 5 October 2012. Retrieved 29 January 2012.
- Mohan, J. (2014), World Drug Report 2014, United Nations Office on Drugs and Crime, retrieved 18 August 2014.
- PubChem – Amphetamine, National Center for Biotechnology Information, retrieved 13 October 2013.
- Nestler, E. J., Hyman, S. E., Malenka, R. C. (2009). Molecular neuropharmacology: a foundation for clinical neuroscience (2nd ed ed.). McGraw-Hill Medical. ISBN 9780071481274.
- Miller, G. M. (January 2011). “The Emerging Role of Trace Amine Associated Receptor 1 in the Functional Regulation of Monoamine Transporters and Dopaminergic Activity”. Journal of neurochemistry. 116 (2): 164–176. doi:10.1111/j.1471-4159.2010.07109.x. ISSN 0022-3042.
- Drugbank – Amphetamine targets.
- TA1 receptor | http://www.iuphar-db.org/DATABASE/ObjectDisplayForward?objectId=364.
- Lewin, A. H., Miller, G. M., Gilmour, B. (December 2011). “Trace amine-associated receptor 1 is a stereoselective binding site for compounds in the amphetamine class”. Bioorganic & Medicinal Chemistry. 19 (23): 7044–7048. doi:10.1016/j.bmc.2011.10.007. ISSN 0968-0896.
- Goodman, L. S., Brunton, L. L., Chabner, B., Knollmann, B. C., eds. (2011). Goodman & Gilman’s pharmacological basis of therapeutics (12th ed ed.). McGraw-Hill. ISBN 9780071624428.
- Eiden, L. E., Weihe, E. (January 2011). “VMAT2: a dynamic regulator of brain monoaminergic neuronal function interacting with drugs of abuse: VMAT2 and addiction”. Annals of the New York Academy of Sciences. 1216 (1): 86–98. doi:10.1111/j.1749-6632.2010.05906.x. ISSN 0077-8923.
- DailyMed – ADDERALL XR- dextroamphetamine sulfate, dextroamphetamine saccharate, amphetamine sulfate and amphetamine aspartate capsule, extended release.
- Sinha, A., Lewis, O., Kumar, R., Yeruva, S. L. H., Curry, B. H. (2016). “Adult ADHD Medications and Their Cardiovascular Implications”. Case Reports in Cardiology. 2016: 2343691. doi:10.1155/2016/2343691. ISSN 2090-6404.
- Dolder, P. C., Strajhar, P., Vizeli, P., Hammann, F., Odermatt, A., Liechti, M. E. (7 September 2017). “Pharmacokinetics and Pharmacodynamics of Lisdexamfetamine Compared with D-Amphetamine in Healthy Subjects”. Frontiers in Pharmacology. 8: 617. doi:10.3389/fphar.2017.00617. ISSN 1663-9812.
- Poulton, A. S., Hibbert, E. J., Champion, B. L., Nanan, R. K. H. (25 April 2016). “Stimulants for the Control of Hedonic Appetite”. Frontiers in Pharmacology. 7: 105. doi:10.3389/fphar.2016.00105. ISSN 1663-9812.
- Nelson, P. E., Moffat, A. C. “Amphetamines and Related Stimulants: Chemical, Biological, Clinical, and Sociological Aspects”. Detection and Identification of Amphetamine and Related Stimulants.
- Biederman, J., Spencer, T. J., Wilens, T. E., Weisler, R. H., Read, S. C., Tulloch, S. J. (December 2005). “Long-term safety and effectiveness of mixed amphetamine salts extended release in adults with ADHD”. CNS spectrums. 10 (12 Suppl 20): 16–25. doi:10.1017/s1092852900002406. ISSN 1092-8529.
- Pigeau, R, Naitoh, P, Buguet, A, McCann, C, Baranski, J, Taylor, M, Thompson, M, MacK, I (December 1995). “Modafinil, d-amphetamine and placebo during 64 hours of sustained mental work. I. Effects on mood, fatigue, cognitive performance and body temperature”. Journal of Sleep Research. 4 (4): 212–228. doi:10.1111/j.1365-2869.1995.tb00172.x. ISSN 1365-2869.
- Broadley, K. J. (1 March 2010). “The vascular effects of trace amines and amphetamines”. Pharmacology & Therapeutics. 125 (3): 363–375. doi:10.1016/j.pharmthera.2009.11.005. ISSN 0163-7258.
- Nutt, D., King, L. A., Saulsbury, W., Blakemore, C. (24 March 2007). “Development of a rational scale to assess the harm of drugs of potential misuse”. The Lancet. 369 (9566): 1047–1053. doi:10.1016/S0140-6736(07)60464-4. ISSN 0140-6736.
- Human health effects – Amphetamine | http://toxnet.nlm.nih.gov/cgi-bin/sis/search/r?dbs+hsdb:@term+@rn+@rel+300-62-9.
- Carvalho, M., Carmo, H., Costa, V. M., Capella, J. P., Pontes, H., Remião, F., Carvalho, F., Bastos, M. de L. (1 August 2012). “Toxicity of amphetamines: an update”. Archives of Toxicology. 86 (8): 1167–1231. doi:10.1007/s00204-012-0815-5. ISSN 1432-0738.
- Miyazaki, I., Asanuma, M. (June 2008). “Dopaminergic neuron-specific oxidative stress caused by dopamine itself”. Acta Medica Okayama. 62 (3): 141–150. doi:10.18926/AMO/30942. ISSN 0386-300X.
- Advokat, C. (July 2007). “Literature Review: Update on Amphetamine Neurotoxicity and Its Relevance to the Treatment of ADHD”. Journal of Attention Disorders. 11 (1): 8–16. doi:10.1177/1087054706295605. ISSN 1087-0547.
- Bowyer, J. F., Hanig, J. P. (14 November 2014). “Amphetamine- and methamphetamine-induced hyperthermia: Implications of the effects produced in brain vasculature and peripheral organs to forebrain neurotoxicity”. Temperature: Multidisciplinary Biomedical Journal. 1 (3): 172–182. doi:10.4161/23328940.2014.982049. ISSN 2332-8940.
- Chetsawang, J., Mukda, S., Srimokra, R., Govitrapong, P., Chetsawang, B. (3 July 2017). “Role of Melatonin in Reducing Amphetamine-Induced Degeneration in Substantia Nigra of Rats via Calpain and Calpastatin Interaction”. Journal of Experimental Neuroscience. 11: 1179069517719237. doi:10.1177/1179069517719237. ISSN 1179-0695.
- Leeboonngam, T., Pramong, R., Sae-Ung, K., Govitrapong, P., Phansuwan-Pujito, P. (April 2018). “Neuroprotective effects of melatonin on amphetamine-induced dopaminergic fiber degeneration in the hippocampus of postnatal rats”. Journal of Pineal Research. 64 (3). doi:10.1111/jpi.12456. ISSN 1600-079X.
- Amphetamine – human health effects | http://toxnet.nlm.nih.gov/cgi-bin/sis/search/a?dbs+hsdb:@term+@DOCNO+3287.
- Amphetamines: Drug Use and Abuse: Merck Manual Home Edition, 2007.
- Pérez-Mañá, C., Castells, X., Torrens, M., Capellà, D., Farre, M. (2 September 2013). Cochrane Drugs and Alcohol Group, ed. “Efficacy of psychostimulant drugs for amphetamine abuse or dependence”. Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD009695.pub2. ISSN 1465-1858.
- “Adderall XR Prescribing Information” | http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/021303s026lbl.pdf.
- Stolerman, I. P., ed. (2010). Encyclopedia of psychopharmacology. Springer. ISBN 9783540687092.
- “Miscellaneous Sympathomimetic Agonists” | http://accessmedicine.mhmedical.com/content.aspx?bookid=374§ionid=41266218&jumpsectionID=41268855.
- Shoptaw, S. J., Kao, U., Ling, W. (21 January 2009). Cochrane Drugs and Alcohol Group, ed. “Treatment for amphetamine psychosis”. Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD003026.pub3. ISSN 1465-1858.
- Hofmann, F. G. (1983). A handbook on drug and alcohol abuse: the biomedical aspects (2nd ed ed.). Oxford University Press. ISBN 9780195030563.
- http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/021303s026lbl.pdf.
- Greenwald, M. K., Lundahl, L. H., Steinmiller, C. L. (December 2010). “Sustained Release d-Amphetamine Reduces Cocaine but not ‘Speedball’-Seeking in Buprenorphine-Maintained Volunteers: A Test of Dual-Agonist Pharmacotherapy for Cocaine/Heroin Polydrug Abusers”. Neuropsychopharmacology. 35 (13): 2624–2637. doi:10.1038/npp.2010.175. ISSN 0893-133X.
- Siciliano, C. A., Saha, K., Calipari, E. S., Fordahl, S. C., Chen, R., Khoshbouei, H., Jones, S. R. (10 January 2018). “Amphetamine Reverses Escalated Cocaine Intake via Restoration of Dopamine Transporter Conformation”. The Journal of Neuroscience. 38 (2): 484–497. doi:10.1523/JNEUROSCI.2604-17.2017. ISSN 0270-6474.
- Krystal, J. H., Perry, E. B., Gueorguieva, R., Belger, A., Madonick, S. H., Abi-Dargham, A., Cooper, T. B., MacDougall, L., Abi-Saab, W., D’Souza, D. C. (1 September 2005). “Comparative and Interactive Human Psychopharmacologic Effects of Ketamine and Amphetamine: Implications for Glutamatergic and Dopaminergic Model Psychoses and Cognitive Function”. Archives of General Psychiatry. 62 (9): 985. doi:10.1001/archpsyc.62.9.985. ISSN 0003-990X.
- “CONVENTION ON PSYCHOTROPIC SUBSTANCES 1971” (PDF). United Nations. Retrieved December 19, 2019.
- “POISONS STANDARD DECEMBER 2019”. Office of Parliamentary Counsel. Retrieved December 19, 2019.
- Controlled Drugs and Substances Act | http://laws-lois.justice.gc.ca/eng/acts/C-38.8/page-24.html#h-28.
- “Sechste Verordnung über die Unterstellung weiterer Stoffe unter die Bestimmungen des Opiumgesetzes” (in German). Reichsministerium des Innern. Retrieved December 25, 2019.
- “Anlage III BtMG” (in German). Bundesministerium der Justiz und für Verbraucherschutz. Retrieved December 19, 2019.
- UNODC – Bulletin on Narcotics – 1957 Issue 3 – 002.
- Règlement grand-ducal du 20 mars 1974 concernant certaines substances psychotropes.
- “Opiumwet” (in Dutch). Ministerie van Binnenlandse Zaken en Koninkrijksrelaties. Retrieved December 19, 2019.
- “Schedule 2 – Class B controlled drugs”. Parliamentary Counsel Office. Retrieved December 19, 2019.
- Läkemedelsverkets föreskrifter (LVFS 1997:12) om förteckningar över narkotika, konsoliderad version till och med LVFS 2010:1.
- “Verordnung des EDI über die Verzeichnisse der Betäubungsmittel, psychotropen Stoffe, Vorläuferstoffe und Hilfschemikalien” (in German). Bundeskanzlei [Federal Chancellery of Switzerland]. Retrieved January 1, 2020.
- Thai Narcotic Act of 2012 | http://narcotic.fda.moph.go.th/faq/upload/Thai%20Narcotic%20Act%202012.doc._37ef.pdf.
- Misuse of Drugs Act 1971.
- Controlled Drugs and Substances Act | http://www.fda.gov/regulatoryinformation/legislation/ucm148726.htm.