Summary
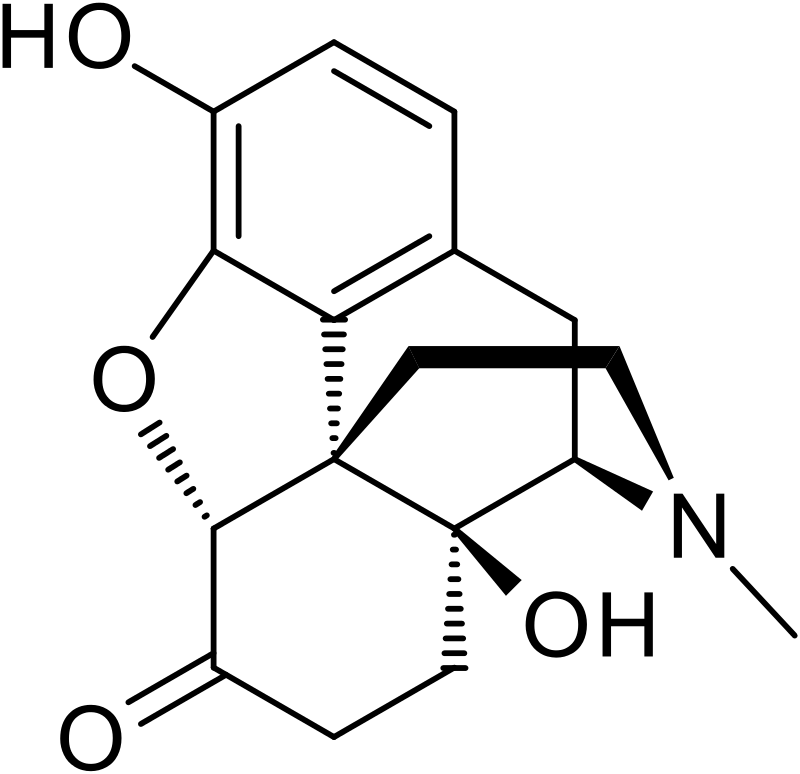
Oxymorphone, commonly recognized under the brand name Opana, is a semi-synthetic opioid analgesic employed for the treatment of moderate to severe pain. It shares a structural resemblance with other opioids like morphine and heroin. Oxymorphone’s origins trace back to its development in Germany in 1914, and it was later introduced to the American market in 1959. Notably, in contrast to many other opioids, oxymorphone lacks significant antitussive properties. Additionally, it plays a vital role as a precursor for other opioids and opioid antagonists, including naloxone.
| Identifiers | |
|---|---|
| IUPAC name | |
| CAS Number | 76-41-5 |
|---|---|
| PubChem CID | 5284604 |
| IUPHAR/BPS | 7094 |
| DrugBank | DB01192 |
| ChemSpider | 4447650 |
| UNII | 9VXA968E0C |
| KEGG | D08323 |
| ChEMBL | ChEMBL963 |
| CompTox Dashboard (EPA) | DTXSID5023409 |
| ECHA InfoCard | 100.000.873 |
| Chemical and physical data | |
| Formula | C17H19NO4 |
| Molar mass | 301.342 g·mol−1 |
Chemistry
Oxymorphone belongs to the morphinan class of opioids, characterized by a polycyclic core comprising three benzene rings fused in a zig-zag pattern, known as phenanthrene. A fourth ring, containing nitrogen, is fused to phenanthrene at positions R9 and R13, with the nitrogen element positioned at R17 within this composite structure, giving rise to the term “morphinan.”
Oxymorphone hydrochloride exists as odorless white crystals or white to off-white powder. Upon prolonged exposure to light, it undergoes darkening in color. Oxymorphone hydrochloride exhibits solubility in water, with one gram dissolving in 4 ml of water, while it is sparingly soluble in alcohol and ether. Notably, it undergoes degradation upon contact with light.
Similar to morphine, hydromorphone, and several other opioids, oxymorphone can undergo acetylation. During the 1930s, mono-, di-, tri-, and tetra-esters of oxymorones were developed, but they are not currently utilized in medical practice.
Pharmacology
Oxymorphone functions by binding to and activating the μ-opioid receptor as an agonist, thereby exerting its effects. This mechanism is rooted in the structural resemblance of opioids to endogenous endorphins. Endorphins, naturally occurring in the body, play a role in analgesia (pain reduction), inducing drowsiness and generating sensations of pleasure. These endorphins can be released in response to various stimuli, including pain, vigorous physical activity, orgasm, or heightened excitement.
Oxymorphone, a semi-synthetic narcotic analgesic closely related to hydromorphone, operates by engaging specific opiate receptors within the central nervous system and smooth muscles. Both hydromorphone and oxymorphone are semi-synthetic derivatives of morphine, possessing potent opiate agonist properties, and are primarily employed in the treatment of moderate-to-severe pain. These effects stem from the opioid’s ability to mimic the actions of endorphins, which include pain alleviation, sedation, and the induction of pleasurable sensations, all of which can be naturally triggered by pain, vigorous physical exertion, orgasm, or heightened emotional arousal.
Subjective effects
Important Note
The effects outlined below are based on the Subjective Effect Index (SEI), which relies on open research literature comprising anecdotal user accounts and personal evaluations by contributors at PsychonautWiki. Therefore, it is prudent to approach these effects with a degree of caution and skepticism.
Additionally, it’s essential to recognize that these effects may not always manifest predictably or consistently. Higher doses are more likely to encompass the entire range of effects, but escalating doses also heighten the risk of adverse outcomes, including addiction, severe harm, or even fatality ☠.
Physical:
- Euphoria: When compared to other opioids, this substance exhibits physical euphoria similar to that of morphine or diacetylmorphine (heroin) and surpasses that of kratom and hydrocodone. It manifests as intense feelings of physical comfort, warmth, affection, and bliss.
- Constipation
- Decreased Libido
- Difficulty Urinating
- Itchiness
- Nausea
- Pain Relief
- Pupil Constriction
- Respiratory Depression
- Sedation
- Skin Flushing
- Appetite Suppression
- Orgasm Suppression
Cognitive:
- Euphoria: Comparable to morphine or diacetylmorphine (heroin) in terms of cognitive euphoria, this substance produces more intense effects than kratom and hydrocodone. It elicits powerful and overwhelming emotions of emotional bliss, contentment, and happiness.
- Anxiety Suppression
- Compulsive Redosing
- Dream Potentiation
Visual:
- Internal Hallucination: At high doses, individuals may enter a state of semi-consciousness and hypnagogia, leading to dream-like states and imagery at up to level 3 intensity. Indistinct geometric patterns often accompany this experience.
Toxicity
Important Safety Information: Risks and Interactions
Please note that unadulterated oxymorphone, like most opioids, typically poses few long-term complications aside from potential dependence and constipation. Nevertheless, the safe use of oxymorones necessitates responsible administration to avoid harmful or toxic effects, including overdose and the use of impure products.
Respiratory Depression and Anoxia:
At heavy dosages, oxymorphone can lead to respiratory depression, potentially resulting in fatal or dangerous levels of oxygen deprivation (anoxia). This occurs due to the suppression of the breathing reflex, which intensifies with higher doses as it corresponds to µ-opioid receptor agonism.
Nausea and Vomiting:
Oxymorphone use may induce nausea and vomiting, which can contribute to fatal opioid overdoses. In such cases, unconscious individuals may aspirate vomit, leading to suffocation. This risk can be mitigated by ensuring that an individual lies on their side with their head tilted downward, preventing airway blockage in case of unconscious vomiting (commonly known as the recovery position).
Opioid Overdose Treatment:
Opioid overdoses can be life-threatening. If you suspect an overdose, immediately call your local emergency number and administer an opioid antagonist such as naloxone.
Tolerance and Addiction Potential:
Oxymorphone, like other opiate-based painkillers, can be highly addictive and may result in both physical and psychological dependence with chronic use. Abrupt discontinuation may lead to withdrawal symptoms.
Tolerance Development:
Prolonged oxymorphone use typically leads to tolerance, reducing the therapeutic effects. This necessitates escalating doses to achieve the same effects. Notably, tolerance to constipation-inducing effects develops particularly slowly. Oxymorphone also exhibits cross-tolerance with all other opioids, diminishing their effects.
Risk After Cessation and Relapse:
Fatal opioid overdoses pose a significantly increased risk after periods of abstinence and relapse due to reduced tolerance. When relapsing, it is safer to administer a fraction of the usual dose to account for this diminished tolerance. Furthermore, the environment plays a role in opioid tolerance; studies have shown that an unfamiliar environment can increase the risk of overdose.
Dangerous Interactions:
Oxymorphone should not be combined with other depressants, as many overdose-related fatalities result from interactions with substances such as alcohol or benzodiazepines. These interactions can lead to dangerously heightened levels of respiratory depression.
Warning: Numerous psychoactive substances, generally safe when used individually, can become difficult or life-threatening when combined with specific other substances. While the following list includes known dangerous interactions, it may not encompass all possibilities. Always conduct independent research to ensure the safety of combining two or more substances, and consult credible sources such as Google, DuckDuckGo, or PubMed. Some of the interactions listed have been sourced from TripSit.
- Alcohol: Combining oxymorphone with alcohol can potentiate ataxia and sedation, potentially causing unexpected loss of consciousness at high doses. Victims should be placed in the recovery position to prevent aspiration from excess vomiting, and memory blackouts are likely.
- Amphetamines: Stimulants increase respiration rate, allowing for higher opioid doses. However, if the stimulant’s effects wear off first, the opioid may overpower the user, leading to respiratory arrest.
- Benzodiazepines: Combining benzodiazepines with oxymorphone can result in central nervous system and respiratory-depressant effects. These substances strongly and unpredictably potentiate each other, rapidly causing unconsciousness. Victims should be placed in the recovery position, and memory loss and blackouts are likely.
- Cocaine: Stimulants elevate respiration rate, permitting higher opioid doses. If cocaine’s effects dissipate first, the opioid may cause respiratory arrest.
- DXM: Generally considered toxic, combining DXM with oxymorphone can lead to central nervous system depression, breathing difficulties, heart issues, and liver toxicity. Additionally, DXM may lower opioid tolerance slightly, causing additional synergistic effects.
- GHB/GBL: Both substances can strongly and unpredictably potentiate each other, rapidly inducing unconsciousness. While unconscious, the risk of aspiration from vomiting exists.
- Ketamine: Both substances carry the risk of vomiting and unconsciousness. If an individual becomes unconscious under the influence, there is a severe risk of aspiration if they are not placed in the recovery position.
- MAOIs: Co-administration of monoamine oxidase inhibitors (MAOIs) with certain opioids can lead to rare reports of severe adverse reactions. These interactions can result in either excitatory or depressive responses, with symptoms ranging from agitation and seizures to coma and death.
- MXE: MXE can potentiate opioid effects but also increase the risk of respiratory depression and organ toxicity.
- Nitrous: Combining nitrous oxide with oxymorphone can potentiate ataxia and sedation, possibly causing unexpected loss of consciousness at high doses. While unconscious, aspiration from vomiting is a risk if the individual is not placed in the recovery position. Memory blackouts are common.
- PCP: PCP may reduce opioid tolerance, increasing the risk of overdose.
- Tramadol: Combining tramadol with oxymorphone can elevate the risk of seizures. Tramadol itself is known to induce seizures and may have additive effects on seizure threshold with other opioids. Additionally, central nervous system and respiratory-depressant effects can be additively or synergistically present.
- Grapefruit: While not psychoactive, grapefruit can influence the metabolism of specific opioids, including oxycodone and fentanyl, by inhibiting the CYP3A4 enzyme. This may prolong the drug’s duration in the body and increase toxicity with repeated doses. Methadone may also be affected. CYP2D6 metabolizes codeine and hydrocodone, and individuals on medications that inhibit CYP2D6 or lack the enzyme due to a genetic mutation may not respond to codeine as it cannot be metabolized into its active product, morphine.
It is strongly advised to prioritize harm reduction practices when using this drug and to exercise utmost caution when considering its interactions with other substances.
Legal status
Certainly, here are the legal status details of oxymorphones in different countries:
- Germany: Oxymorphone is classified as a controlled substance under BtMG Anlage II, making it illegal to manufacture, import, possess, sell, or transfer without a license.
- Russia: Oxymorphone is categorized as a Schedule I controlled substance.
- Switzerland: Oxymorphone is considered a controlled substance and is specifically listed under Verzeichnis A. Medicinal use is permitted.
- United Kingdom: Oxymorphone is classified as a Class A, Schedule 2 drug in the United Kingdom.
- United States: In the United States, oxymorphone is designated as a Schedule II Controlled Substance.
FAQ
- What is Oxymorphone?
- Oxymorphone is a potent opioid analgesic used for managing moderate to severe pain. It belongs to the opioid class of drugs and is known by the brand name Opana.
- How does Oxymorphone work?
- Oxymorphone works by binding to and activating the μ-opioid receptors in the brain and spinal cord. This action results in pain relief and feelings of euphoria and relaxation.
- Is Oxymorphone the same as other opioids like morphine or heroin?
- Oxymorphone is similar in structure to other opioids like morphine and heroin. However, it has its unique characteristics and effects.
- When was Oxymorphone first developed?
- The oxymorphone was first developed in Germany in 1914 and introduced to the American market in 1959.
- What are the common medical uses of Oxymorphone?
- Oxymorphone is primarily prescribed to manage moderate to severe pain, especially in cases where other pain medications are not effective.
- What are the potential side effects of Oxymorphone use?
- Common side effects may include constipation, nausea, vomiting, respiratory depression, and sedation. It can also lead to dependence and addiction if not used as prescribed.
- Is Oxymorphone legal?
- The legal status of oxymorphones varies by country. In some places, it is controlled as a prescription medication, while in others, it is classified as an illegal substance.
- Can Oxymorphone be dangerous?
- Yes, oxymorones can be dangerous, especially when misused or combined with other substances like alcohol or benzodiazepines. It can lead to respiratory depression and overdose.
- How can Oxymorphone overdose be treated?
- Oxymorphone overdose can be treated by administering an opioid antagonist like naloxone. In case of an overdose, seek immediate medical attention.
- Is Oxymorphone addictive?
- Yes, oxymorphones can be highly addictive, both physically and psychologically. Prolonged use can lead to tolerance, dependence, and withdrawal symptoms when usage is stopped.
- What precautions should I take when using Oxymorphone?
- It is essential to use Oxymorphone only as prescribed by a healthcare professional. Follow the recommended dosage, and do not mix it with other substances without medical advice.
- Can I legally purchase Oxymorphone online?
- Purchasing Oxymorphone online without a valid prescription is illegal in most countries and can be dangerous due to the risk of counterfeit or impure products.
- What should I do if I suspect someone is experiencing an Oxymorphone overdose?
- If you suspect someone is overdosing on Oxymorphone, call emergency services immediately. While waiting for help, try to keep the person awake and breathing if possible.
References
- Sinatra, R. S., Jahr, J. S., Watkins-Pitchford, J. M., eds. (2010). “The Essence of Analgesia and Analgesics.” This comprehensive resource delves into the world of analgesia and its essential components. It provides valuable insights into pain management. (doi:10.1017/CBO9780511841378)
- Davis, M. P., Glare, P. A., Hardy, J., Quigley, C., eds. (May 2009). “Opioids in Cancer Pain.” This publication explores the use of opioids in the context of cancer pain management, shedding light on their role and efficacy. (doi:10.1093/med/9780199236640.001.0001)
- Brayfield, A. (3 September 2014). Soni, H., ed. “‘Oxymorphone Hydrochloride.’ Martindale: The Complete Drug Reference.” This entry in Martindale’s authoritative drug reference provides valuable information about oxymorphone hydrochloride, aiding in understanding its properties and uses. (Pharmaceutical Press. 22 (5). doi:10.7748/en.22.5.12.s13)
- Merck Manual of Home Health Handbook – 2nd edition, 2003, p. 2097. This edition of the Merck Manual of Home Health Handbook offers a wealth of health-related information, including insights into various medical topics.
- “Why Heroin Relapse Often Ends In Death” – Lauren F Friedman (Business Insider). This article from Business Insider explores the grim reality of heroin relapse and its often fatal consequences. (http://www.businessinsider.com.au/philip-seymour-hoffman-overdose-2014-2)
- Siegel, S., Hinson, R. E., Krank, M. D., McCully, J. (23 April 1982). “Heroin ‘Overdose’ Death: Contribution of Drug-Associated Environmental Cues.” In this scientific study, the factors contributing to heroin overdose deaths, including environmental cues, are examined. (Science. 216 (4544). doi:10.1126/science.7200260)
- Darke, S., Zador, D. (December 1996). “Fatal heroin ‘overdose’: a review.” This review in Addiction delves into the topic of fatal heroin overdose, shedding light on the factors involved. (91 (12). doi:10.1046/j.1360-0443.1996.911217652.x)
- Ershad, M., Cruz, M. D., Mostafa, A., Mckeever, R., Vearrier, D., Greenberg, M. I. (March 2020). “Opioid Toxidrome Following Grapefruit Juice Consumption in the Setting of Methadone Maintenance.” This research in the Journal of Addiction Medicine explores the occurrence of opioid toxidrome linked to grapefruit juice consumption. (14 (2). doi:10.1097/ADM.0000000000000535)
- Anlage II BtMG – Einzelnorm. This legal reference provides information on the controlled status of substances in Germany, including oxymorphone.
- Постановление Правительства РФ от 01.10.2012 N 1002 (ред. от 09.08.2019). This Russian government decree outlines the regulatory framework related to controlled substances in Russia.
- “Verordnung des EDI über die Verzeichnisse der Betäubungsmittel, psychotropen Stoffe, Vorläuferstoffe und Hilfschemikalien” (in German). This document from the Federal Chancellery of Switzerland pertains to the classification of substances, including oxymorphone, in Switzerland.
- List of most commonly encountered drugs currently controlled under the misuse of drugs legislation. This list provides an overview of commonly encountered drugs that are controlled under drug misuse legislation.
- Drug Enforcement Administration Controlled Substances. This resource offers information on substances classified as controlled by the Drug Enforcement Administration in the United States. (https://www.deadiversion.usdoj.gov/schedules/orangebook/e_cs_sched.pdf)