Contents
Summary
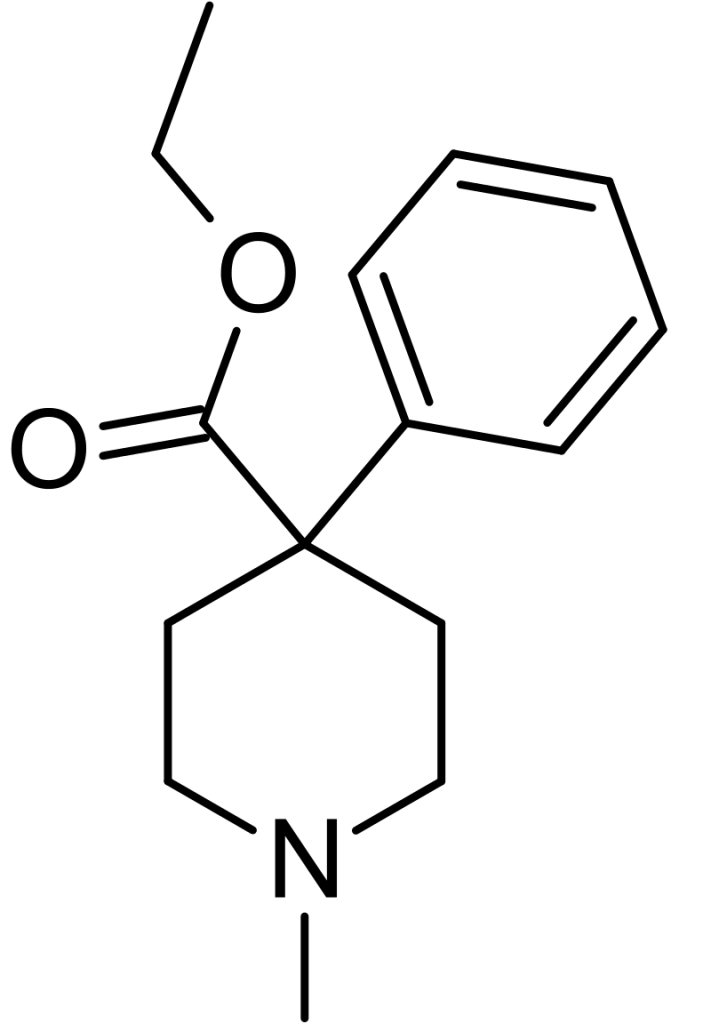
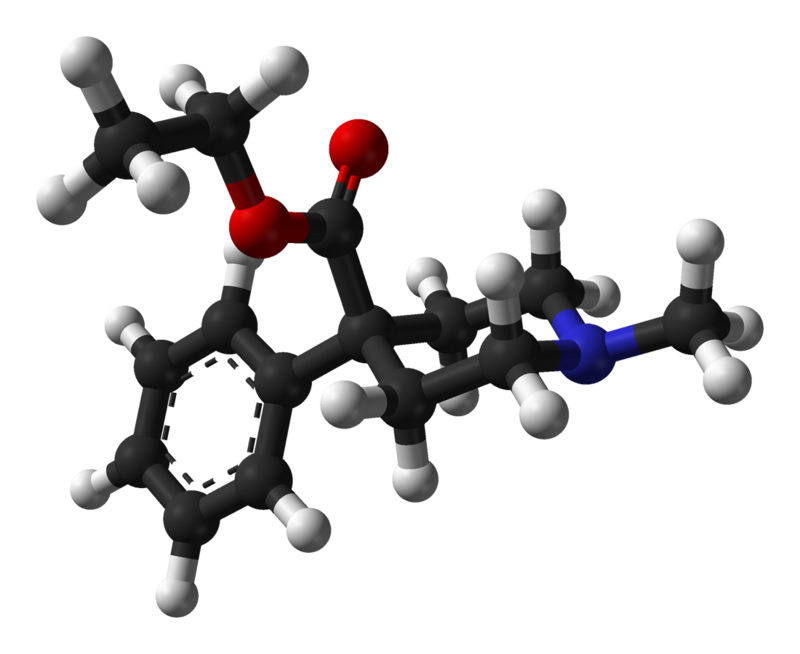
Pethidine, also recognized as meperidine and marketed under the trade name Demerol and other brands, is a synthetic opioid analgesic belonging to the phenylpiperidine class. It was synthesized in 1938[10] with the initial intention of being an anticholinergic agent, a project led by the German chemist Otto Eisler. However, its pain-relieving properties were later identified by Otto Schaumann during his tenure with IG Farben in Germany. Pethidine serves as the archetype for a substantial group of pain relievers, including 4-phenylpiperidine derivatives (such as piminodine and anileridine), prodines (alphaprodine, MPPP, etc.), bemidones (ketobemidone, etc.), and other more distantly related compounds like diphenoxylate and its analogs.
Pethidine is primarily prescribed for the management of moderate to severe pain. It is available in various forms, including tablets as a hydrochloride salt, as a syrup, or for administration through intramuscular, subcutaneous, or intravenous injection. Throughout a significant portion of the 20th century, pethidine was the opioid of choice for many healthcare professionals. In 1975, approximately 60% of doctors prescribed it for acute pain, while 22% prescribed it for chronic severe pain.
Pethidine was initially patented in 1937 and gained approval for medical use in 1943. Initially, it was believed to be a safer alternative to morphine, carrying a lower risk of addiction, and was considered superior in treating pain associated with conditions like biliary spasm or renal colic due to its purported anticholinergic properties. However, subsequent research revealed these assumptions to be inaccurate. Pethidine presents an equal risk of addiction, offers no significant advantages in addressing biliary spasms or renal colic when compared to other opioids, and, due to the formation of a toxic metabolite called norpethidine, it exhibits greater toxicity, especially during prolonged use. Additionally, it was discovered that norpethidine has serotonergic effects, making pethidine unique among most opioids as it can potentially contribute to serotonin syndrome.
| Identifiers | |
|---|---|
| IUPAC name | |
| CAS Number | 57-42-1 |
|---|---|
| PubChem CID | 4058 |
| IUPHAR/BPS | 7221 |
| DrugBank | DB00454 |
| ChemSpider | 3918 |
| UNII | 9E338QE28F |
| KEGG | D08343 |
| ChEBI | CHEBI:6754 |
| ChEMBL | ChEMBL607 |
| CompTox Dashboard (EPA) | DTXSID9023253 |
| ECHA InfoCard | 100.000.299 |
| Chemical and physical data | |
| Formula | C15H21NO2 |
| Molar mass | 247.338 g·mol−1 |
Chemistry
Pethidine, belonging to the phenylpiperidine class of synthetic opioids, serves as the prototype for a diverse group of analgesic compounds. This extensive family includes pethidine 4-phenylpiperidines like piminodine and anileridine, prodines such as alphaprodine and MPPP, besides including ketobemidone, and other more distantly related compounds like diphenoxylate and its analogues. In its hydrochloride form, pethidine typically appears as a white crystalline substance with a melting point ranging from 186°C to 189°C. It exhibits high solubility in water, possesses a neutral pH, and carries a slightly bitter taste.
Regarding its toxicity, a concentration of 500 micrograms per deciliter (ug/dL) is considered toxic in the bloodstream. In contrast, a lethal concentration typically falls within 1-3 milligrams per deciliter (mg/dL).
The synthesis of pethidine involves a two-step process. Initially, benzyl cyanide and chlormethine are reacted in the presence of sodium amide to yield a piperidine ring. Subsequently, the nitrile group is converted into an ester.
Pharmacology
Opioids achieve their effects by binding to and activating the μ-opioid receptor. This mechanism is possible because opioids structurally resemble endogenous endorphins, naturally occurring in the body and engaging the μ-opioid receptor. This structural similarity underlies the euphoria, pain relief, and anxiolytic (anxiety-reducing) effects of opioids. Endorphins are crucial in diminishing pain, inducing drowsiness, and eliciting pleasurable sensations. They are released in response to various stimuli, including pain, strenuous physical activity, orgasm, or moments of excitement.
Regarding orally administered pethidine, its bioavailability can range from 50% to approximately 60%.
Pethidine exhibits a notably distinctive pharmacological profile compared to conventional opioids. Apart from its opioid properties, pethidine also functions as an antagonist for muscarinic acetylcholine receptors. Furthermore, it acts as a dopamine reuptake inhibitor and a norepinephrine reuptake inhibitor. Additionally, pethidine serves as an agonist for κ-opioid receptors, and its metabolite, norpethidine, possesses remarkable potency as a serotonin reuptake inhibitor.
Subjective effects
Disclaimer: The effects listed below are based on anecdotal user reports and the personal analyses of contributors from the Subjective Effect Index (SEI), an open research literature. Therefore, it is advisable to approach them with a healthy degree of scepticism.
It’s important to note that these effects may not necessarily occur predictably or reliably, although higher doses are more likely to encompass the full range of products. Additionally, it should be understood that adverse effects become increasingly likely at higher doses and may include risks such as addiction, severe injury, or even death ☠. Many users have reported perceiving pethidine as being just as, or even more euphoric than, oxycodone.
Physical:
- The overall sensation associated with pethidine can be described as euphoria, relaxation, anxiety relief, and pain alleviation.
- Pain relief
- Physical euphoria: Pethidine is particularly intense in its physical euphoric effects, characterized by profound sensations of material comfort, warmth, love, and bliss.
- Itchiness
- Respiratory depression: At low to moderate doses, this effect may mildly to moderately slow down breathing without significant impairment. However, high doses and overdoses can lead to opioid-induced respiratory depression, resulting in breathlessness, abnormal breathing patterns, semi-consciousness, or unconsciousness. Severe overdoses can lead to a coma or death without immediate medical intervention.
- Constipation
- Cough suppression
- Difficulty urinating
- Nausea
- Sedation or Stimulation: While most users consider pethidine sedating, some find it stimulating.
- Pupil constriction
- Decreased libido
- Appetite suppression
- Orgasm suppression
- Seizures: High doses of pethidine may provoke seizures due to its metabolite, norpethidine.
Cognitive:
- Cognitive euphoria: Pethidine’s mental delight is notably intense, described as a powerful and overwhelming sense of emotional bliss, contentment, and happiness.
- Anxiety suppression
- Compulsive redosing
- Dream potentiation
Visual:
- Acuity suppression: Pethidine, acting as a muscarinic acetylcholine receptor antagonist, may lead to blurred vision, especially at high doses.
Toxicity
Pethidine carries a relatively high toxicity relative to its dose. Like all opioids, its long-term effects can vary but may encompass reduced libido, apathy, and memory impairment. Combining it with depressants such as alcohol or benzodiazepines can be potentially lethal, and it generally presents a broader range of substances that can be dangerous when combined compared to other opioids.
One of pethidine’s metabolites, norpethidine, lacks significant opioid activity but is known to trigger seizures. Therefore, it is crucial to avoid taking pethidine during benzodiazepine withdrawals, as this combination may potentially induce seizures.
In a tragic case from 1984, a teenager named Libby Zion was admitted to the emergency room with flu-like symptoms. She was previously prescribed and taking phenelzine, a monoamine oxidase inhibitor. The combination of these medications led to fatal serotonin syndrome.
It is strongly advised to practice harm reduction when using this drug.
Tolerance and Addiction Potential
Pethidine, like other opioids, can be highly addictive, with substantial potential for abuse, leading to psychological dependence in certain users. Those addicted may experience cravings and withdrawal symptoms if they suddenly cease using it.
Tolerance to various effects of pethidine develops over time with repeated use. Different products may develop tolerance at varying rates, with constipation-inducing effects developing particularly slowly. Consequently, users may need to increase their doses significantly to achieve the same impact. Patience typically takes 3 to 7 days to decrease by half and 1 to 2 weeks to return to baseline (without further consumption). Pethidine also exhibits cross-tolerance with all other opioids, meaning that after using pethidine, the effects of all opioids will be reduced.
The risk of fatal opioid overdoses increases significantly after cessation and relapse due to reduced tolerance.[8] To mitigate this risk, it is safer to administer only a fraction of the usual dosage if relapsing. Additionally, the environment in which the opioid is consumed may affect tolerance. A scientific study on rats showed that those with a history of heroin administration were significantly more likely to die if they received their dose in an unfamiliar environment compared to a familiar one.
Dangerous Interactions
Warning: Combining psychoactive substances considered reasonably safe can become dangerous or even life-threatening. The following list includes some known dangerous interactions, although it may not cover all.
Always conduct independent research (e.g., through Google, DuckDuckGo, PubMed) to ensure the safety of combining two or more substances. Some of the listed interactions have been sourced from TripSit.
- Alcohol: Both substances potentiate each other’s ataxia and sedation, potentially leading to sudden loss of consciousness, especially at high doses. Affected individuals should be placed in the recovery position to prevent aspiration of vomit, and memory blackouts are likely.
- Amphetamines: Stimulants increase respiration rate, allowing for higher opioid doses than would otherwise be used. However, if the stimulant effects wear off first, the opioid may overpower the user, causing respiratory arrest.
- Benzodiazepines: Central nervous system and respiratory depressant effects may be additive or synergistic, rapidly leading to unconsciousness. While unconscious, there is a risk of vomit aspiration if the individual is not placed in recovery, and blackouts/memory loss are common.
- Cocaine: Stimulants increase respiration rate, enabling higher opioid doses than usual. However, if the stimulant wears off before the opioid, it may lead to respiratory arrest.
- DXM: Generally considered toxic, combining DXM with opioids can result in central nervous system depression, breathing difficulties, heart issues, and liver toxicity. Additionally, taking DXM can lower opioid tolerance, potentially enhancing synergistic effects.
- GHB/GBL: These substances intensely and unpredictably potentiate each other, rapidly inducing unconsciousness. While unconscious, there is a risk of vomit aspiration if the person is not placed in recovery.
- Ketamine: Both substances carry a risk of vomiting and unconsciousness. Suppose the user loses consciousness while under the influence; there is a severe risk of vomit aspiration if they are not placed in the recovery position.
- MAOIs: Co-administration of monoamine oxidase inhibitors (MAOIs) with certain opioids has been linked to rare cases of severe adverse reactions. These reactions can be excitatory or depressive. Symptoms may include agitation, headache, sweating, hyperpyrexia, flushing, shivering, myoclonus, rigidity, tremors, diarrhoea, high blood pressure, rapid heart rate, seizures, and coma. In some instances, death has occurred.
- MXE: While MXE can potentiate opioid effects, it also increases the risk of respiratory depression and organ toxicity.
- Nitrous: Both substances potentiate each other’s ataxia and sedation, potentially leading to sudden loss of consciousness, especially at high doses. While unconscious, there is a risk of vomit aspiration if the individual is not placed in recovery, and memory blackouts are common.
- PCP: PCP may reduce opioid tolerance, increasing the risk of overdose.
- Tramadol: There is an increased risk of seizures when combining tramadol with other opioids. Tramadol is known to induce seizures and may have additive effects on seizure threshold when combined with other opioids. Central nervous system and respiratory-depressant impact may also be additively or synergistically present.
- Grapefruit: While not psychoactive, grapefruit can affect the metabolism of certain opioids. Drugs like tramadol, oxycodone, and fentanyl are primarily metabolized by the enzyme CYP3A4, which is strongly inhibited by grapefruit juice. This can prolong drug clearance from the body, potentially increasing toxicity with repeated doses. Methadone may also be affected. CYP2D6 metabolizes codeine and hydrocodone, and individuals taking medications that inhibit CYP2D6 or lack the enzyme due to a genetic mutation will not respond to codeine because it cannot be metabolized into its active form, morphine.
Serotonin Syndrome Risk
Pethidine has a significantly higher risk of causing serotonin syndrome than other serotonergic opioids, such as tramadol.[citation needed] Combining pethidine with the following substances can result in dangerously high serotonin levels. Serotonin syndrome requires immediate medical attention and can be fatal if left untreated.
- MAOIs: Examples include banisteriopsis caapi, Syrian rue, phenelzine, selegiline, and moclobemide.
- Serotonin releasers: Such as MDMA, 4-FA, methamphetamine, methylone, and αMT.
- SSRIs: Such as citalopram and sertraline.
- SNRIs: Such as tramadol and venlafaxine.
- 5-HTP
Legal status
Germany: Pethidine is a controlled substance under Anlage III of the BtMG and can only be prescribed using a narcotic prescription form.
Russia: Pethidine is categorized as a Schedule I controlled substance.
Switzerland: Pethidine is listed as a controlled substance in Verzeichnis A, with medicinal use permitted.
Turkey: Pethidine is classified as a ‘red prescription’ only substance and is illegal to sell or possess without a prescription.[citation needed]
United Kingdom: Pethidine is classified as a Class A, Schedule 2 drug in the United Kingdom.
United States: Pethidine is designated as a Schedule II Controlled Substance.
FAQ
1. What is Pethidine?
- Pethidine, also known as meperidine in the United States, is a synthetic opioid medication. It is primarily used for treating moderate to severe pain and is classified as a narcotic analgesic.
2. How does Pethidine work?
- Pethidine works by binding to and activating the μ-opioid receptors in the brain and spinal cord. This action leads to pain relief and other opioid-related effects, such as euphoria and sedation.
3. What conditions is Pethidine prescribed for?
- Pethidine is commonly prescribed for pain management, including post-surgical pain, labour pain, and certain medical conditions causing severe pain.
4. Is Pethidine safe to use?
- Pethidine can be safe and effective when used as prescribed by a healthcare professional. However, like all opioids, it carries potential risks, including addiction, respiratory depression, and overdose, if not used as directed.
5. What are the potential side effects of Pethidine?
- Common side effects of Pethidine include drowsiness, constipation, nausea, vomiting, and dizziness. It can also cause more severe side effects like respiratory depression, allergic reactions, and seizures in some cases.
6. Is Pethidine addictive?
- Yes, Pethidine has a high potential for addiction and dependence, mainly when used for extended periods or at higher doses than prescribed. It is essential to use it only as directed by a healthcare provider.
7. Can Pethidine be used during pregnancy?
- Pethidine is sometimes used during labour to relieve pain. However, its use during pregnancy should be carefully considered and discussed with a healthcare provider, as it can pass through the placenta and affect the baby.
8. Is Pethidine safe to use with other medications?
- Pethidine can interact with other drugs, including alcohol and certain antidepressants. To avoid potentially harmful interactions, it’s crucial to inform your healthcare provider about all medications and supplements you are taking.
9. Can I drive or operate machinery while taking Pethidine?
- Pethidine can cause drowsiness and impair your ability to drive or operate heavy machinery. It is advisable to avoid such activities until you know how the medication affects you.
10. Is Pethidine available over-the-counter?
- No, Pethidine is a prescription-only medication and cannot be obtained without a prescription from a qualified healthcare provider.
11. What should I do if I suspect someone has overdosed on Pethidine?
- An overdose of Pethidine can be life-threatening and requires immediate medical attention. Call emergency services (911 in the United States) if you suspect an overdose.
12. Can I suddenly stop taking Pethidine?
- Abruptly discontinuing Pethidine after prolonged use can lead to withdrawal symptoms. It is essential to follow your healthcare provider’s guidance when stopping the medication to minimize withdrawal effects.
13. Is Pethidine available under different brand names?
- Pethidine is available under various brand names depending on the region and manufacturer. Some common brand names include Demerol, Pethidor, and Meperidine.
14. Where is Pethidine classified as a controlled substance?
- Pethidine is classified as a controlled substance in many countries, including the United States, Germany, and the United Kingdom. Its legal status and regulations may vary from one region to another.
15. Can I share my Pethidine prescription with someone else?
- No, it is illegal and unsafe to share prescription medications with others. Pethidine should only be used by the person for whom it was prescribed under the guidance of a healthcare provider.
References
- In a 1957 article titled “Morphine & Allied Drugs” in the Journal of the American Pharmaceutical Association (Scientific ed.), the effects and properties of morphine and related substances were discussed, highlighting their significance in the field of pharmacology.
- Information about (+-)-Pethidine hydrochloride, including its uses, side effects, and chemistry, can be found in drug references. This information is crucial for understanding the medication.
- A patent application from IG Farben in 1937 sheds light on the historical development of pharmaceuticals, including pethidine.
- A critical review of meperidine (a medication related to pethidine) was published in the American Journal of Therapeutics in January 2002. This review examined the drug’s properties and potential issues.
- Research conducted in 1999 by Walker and Zacny, published in the Journal of Pharmacology and Experimental Therapeutics, explored the subjective, psychomotor, and physiological effects of opioid μ agonists in healthy volunteers. This study helps to understand the effects of opioids like pethidine.
- The “Libby Zion Affair” and its relation to serotonin syndrome were discussed in an article in Emergency Physicians Monthly in 2011, highlighting the importance of understanding drug interactions.
- An article by Lauren F. Friedman in Business Insider in 2014 discussed why heroin relapse often ends in death, emphasizing the dangers associated with opioids.
- A 1982 study by Siegel et al. in Science explored the environmental cues associated with heroin “overdose” deaths, providing insights into the factors contributing to opioid-related fatalities.
- A case report published in the Journal of Addiction Medicine in March 2020 by Ershad et al. discussed the occurrence of opioid toxidrome following grapefruit juice consumption in the context of methadone maintenance.
- The relationship between monoamine oxidase inhibitors, opioid analgesics, and serotonin toxicity was discussed by Gillman in the British Journal of Anaesthesia in 2005, underscoring the importance of understanding drug interactions.
Legal References
- Anlage III BtMG (Germany) – This legal norm classifies pethidine as a controlled substance in Germany.
- Постановление Правительства РФ (Russia) – This government resolution classifies pethidine as a Schedule I controlled substance in Russia.
- “Verordnung des EDI über die Verzeichnisse der Betäubungsmittel, psychotropen Stoffe, Vorläuferstoffe und Hilfschemikalien” (Switzerland) – This Swiss regulation lists pethidine as a controlled substance and permits its medicinal use.
- KIRMIZI REÇETEYE TABİ İLAÇLAR (Turkey) – In Turkey, pethidine is categorized as a ‘red prescription’ only substance and is illegal without a prescription.
- List of most commonly encountered drugs currently controlled under the misuse of drugs legislation (United Kingdom) – Pethidine is classified as a Class A, Schedule 2 drug in the United Kingdom.
- DEA Controlled Substances (United States) – Pethidine is designated as a Schedule II Controlled Substance in the United States, highlighting its controlled status under federal law.